Nearly three years ago my husband had Total Knee Replacement (TKR) surgery. It’s drastic and major surgery, which people usually only choose when the pain from osteoarthritis becomes intolerable. And, it was not done properly so that last month it had to be re-done! Perhaps our experience can be useful to others.
Why do knees need to be replaced?
Generally because of pain and restricted motion caused by loss of cartilage (which cushions and separates the bony parts of a joint) and growth of bony “spurs”. This is labelled osteoarthritis. Other causes, like trauma, rheumatoid arthritis, and infection, account for a minority of the 300,000+ TKRs each year in the US.
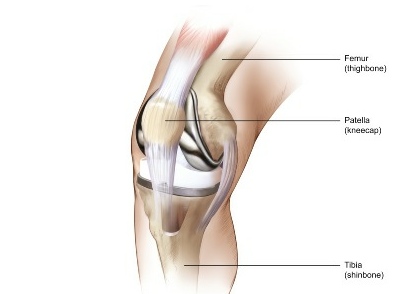
As to what causes osteoarthritis, that is less understood than previously thought, when it was all blamed on “wear and tear”. The knee is the largest joint in the body, and bears the complete weight of the body at each step we take, so it is indeed subject to lots of “wear and tear”. Common-sense risk factors include types of high-stress activity in work or sports, injury, obesity, infection, stiffness from lack of activity, and age (since cartilage becomes more brittle with age). However, not all elderly people develop arthritis and some who do have no significant pain. This is why I said above that knees need to be replaced, not because of osteoarthritis, but because of pain and reduced range of motion.
The biologic factors leading to the deterioration of cartilage in osteoarthritis are not entirely understood. Many experts believe that osteoarthritis results from a genetic susceptibility that causes some biologic response to injuries to the joint, which in turn leads to progressive deterioration of cartilage. In addition, the ability to make repairs becomes progressively limited as cartilage cells age.
Although osteoarthritis generally accompanies aging, osteoarthritic cartilage is chemically different from normal aged cartilage. As chondrocytes (the cells that make up cartilage) age, they lose their ability to make repairs and produce more cartilage. This process may play an important role in the development and progression of osteoarthritis. [Emphasis mine. Source: www.healthcentral.com ]
What’s involved in Total Knee Replacement surgery?
The x-rays below, from the site of a prosthetics manufacturer,

show views of a knee before and after surgery. On the left, cartilage loss has caused bone-on-bone contact: very painful. Bone spurs or bits of broken bone floating around can also cause pain in the deteriorated joint. On the right, an artificial knee joint (prosthesis) is in place. (These are not x-rays of the same knee; in fact, looks to me like one’s a left leg and the other is a right leg.)
Here are some views of prostheses. To install them, the ends of the two long-bones of the leg, tibia and femur, are sawed off (removing “usually between 2 and 12 mm” according to one source) and the artificial joint is affixed with cement, screws, etc. The work involved in removing bone and attaching the prosthesis involves considerable force and power tools. Note that the knee-cap, as well as muscles and ligaments, must be carefully moved aside to install the prosthesis. [Picture sources: 1, 2, 3 ]


There are many patented designs for artificial knee joints, and these illustrations are for general example only. Surgeons have their preferred models; many were developed by orthopedic surgeons, and those surgeons tend to prefer the ones they have an interest in. Choice of prosthesis isn’t something the patient can weigh in on, we don’t know enough, but you may want to find out if your surgeon has a financial interest in the one he is going to use; if so, perhaps a second opinion would be valuable on the pros and cons of various types as applied to your individual case. Most insurance will pay for a second opinion for major surgery.
Research continues for better, longer-lasting designs and breakthroughs are regularly announced with fanfare––but some don’t fulfill their original promise, as with teflon-lined joints which wore away much faster in practice than lab tests had predicted. You will have to rely on the experience of your surgeon.
You can see photos of the stages of knee surgery (not for the faint-hearted) here, on a prosthesis company ‘s site.
Our experience
Surgery #1, 2006
Now, back to my husband’s case. Dan had knee pain for years that ruled out unnecessary walking, as in hiking or walking for enjoyment, and interfered with sleep. There was bone on bone contact and perhaps bone spurs or growths from osteoarthritis. In August 2006 he underwent total knee replacement surgery by an established older orthopedist in our area. Afterwards, the surgeon came out to me in the waiting room and told me that the operation had taken half again as long as planned because they had “run into something unexpected”. Later, when we knew more, that remark would have much more significance to us. The “something unexpected” was apparently the result of a broken leg at age ten, that had caused greater reliance on the other leg (the one that received the TKR).
The surgery was brutal, with terrible bruising all over the leg, and post-op pain and swelling were severe. From the beginning, the prosthesis felt loose and insecure, sometimes the knee buckled, and after the post-surgical pain subsided, he was still in pain sufficient to make walking difficult. At each visit with the surgeon Dan raised these issues and was told to exercise more, and that it would get better with time. Two years on, that hadn’t happened, and the surgeon then agreed that the knee was a bit loose and offered to go back in and “put a shim in it”.
At some point after the 2006 operation, when it became apparent that it had been unsuccessful, I began to research the subject. Immediately I found that it’s common practice now to use Magnetic Resonance Imaging before TKR, rather than merely relying on x-rays. MRIs provide an exact and minutely detailed three-dimensional picture of the joint. The data can be used to make a 3-D visualization that can be rotated. This way the surgeon knows exactly what to expect; the prosthesis is customized, if necessary, beforehand; the surgery is generally shorter and the incision may even be smaller. (Other advances, such as computer-assisted orientation systems to guide the surgeon in positioning the prosthesis during surgery, may also be used.) Nothing like this was done in Dan’s case, and we didn’t know to ask about it. We know now that the original surgeon does have access to an MRI, in the hospital across the street from his office, and used it to look at Dan’s hip after the bad artificial knee began to cause a lot of pain in his hip, back, and other knee. But he didn’t use it for the knee needing replacement.
Surgery #2, 2009
Finally, after the remark about putting in a “shim”, we began to look for another surgeon. I searched online for someone who used MRIs and computerized techniques for joint replacement and who was experienced in what I learned is called “revision” (re-do) of TKRs. (Some surgeons, including the only other ones in our area, won’t touch someone else’s failures.) I found a surgeon who met these qualifications, about 4 hours drive from where we live, and we went to see him. The first thing he did was to get a full-leg digital x-ray, which surgeon #1 had never done. He showed us the x-ray, and used software to examine the precise alignment of the prosthesis. It was 7.5° out of alignment. In effect, his lower leg-bone had been detached and then put back on at a different angle from the upper leg. For over two years the first surgeon had taken no steps to examine the results of his surgery, other than feeling the knee.
We liked what we saw here, added to what we already knew about Surgeon #2’s experience, and proceeded with the preparations for a revision.
In late May Dan went through the revision surgery. Pry off the old, shave off a little more bone, affix the new.
When the surgeon met with me afterward in the waiting room, he had troubling things to report but they weren’t about what had just taken place. He told me that the prosthesis he had removed was badly installed. He actually used the word “sloppy”––and you know how rare it is for doctors to criticize one another’s work! The lower part was out of alignment both front-to-back and side-to-side; the upper part was supposed to be stabilized by the bone growing into it on all sides, but this had not taken place (he remarked that he did not use this model because sufficient bone regrowth often failed to occur). So this artificial joint had been loose and seriously mis-aligned, with every step stressing both parts of the prosthesis, the ends of the bones, the muscles/ligaments/tendons, and the other joints involved in walking (back, hip, other knee). It was clear, said the surgeon, that this had been causing Dan considerable pain, and he felt confident that the new prosthesis was going to be a great improvement.
Today is post-op day 19, and there is no comparison between the two post-op experiences. The day after the surgery they got Dan on his feet, and the first time he put his weight on the new knee he said that it felt more solid than the old one ever had. The next day he was walking the hall, slowly, and walking without hip pain for the first time in ten years. Bruising of the leg is minimal, the incision is shorter, and pain is less. The first time he was using fentanyl patches, very heavy opioid painkiller, and was still in too much pain. This time it is Tylenol-3 every 4 hours, and ultram (tramodol) occasionally when needed.
The incision is closed with superglue, covered with crossways lengths of what looks like strapping tape: no staples to distort the skin and then have to be removed. He was able to take a short shower on post-op day 5. Last time the first shower was not permitted nearly so soon and he was in so much pain he had to sit down on a plastic bench in the shower. This time, he was easily able to stand and feel secure. He’s in pain, but not nearly as much as last time, and the solidity of the knee makes it possible for him to get around the house carefully but confidently, only occasionally using his walking stick for stability (and to keep the dogs from bumping him).
Like the first time, the anesthesia was a spinal block (not general anesthesia) but the new surgeon added a femoral nerve block. As I understand it, the spinal keeps pain messages from reaching the brain during surgery; the femoral block keeps the nerves immediately affected by the surgery from registering pain which gets the nerves excited even though the brain doesn’t hear about it. It’s supposed to lessen post-op pain and it certainly seems to do that, especially for the first 24-36 hours.
There is swelling, but it’s not bad unless he keeps his leg bent too long while sitting; last time he was still mostly in bed for at least 2 weeks, and the swelling was severe from above the knee to the foot. Perhaps this is related to another difference in surgical procedure: this time a drain was placed near the incision with a receptacle attached which had to be periodically emptied of fluid, partly blood. Before the drain was removed, 1200 cc of fluid had been collected. The first surgeon did not place such a drain, the leg continued very swollen, and at the two-week check-up the surgeon had to use a syringe to remove at least 200 cc from the still very swollen knee. Doing this is risky because in raises the risk of infection, which would be a dire complication.
At this point the future looks very good for this new knee, and we are talking about being able to get out and hike with our dogs again. I still have limited energy (fibromyalgia) but more than I used to, since getting off of methadone which I took for pain.
Lessons learned
The parts of our experience that I think may be useful to everybody facing joint replacement surgery are these:
Research and ask questions. Get a second opinion.
This is major surgery which will shape your everyday life for the next decade or more. Revisions are to be avoided: not only because of pain and expense, but each surgery removes a little more bone. Don’t be afraid of getting a second opinion, even if your orthopedic surgeon seems great. Believe me, if your orthopedist were going in for brain or heart surgery, he or she would ask around, not just take the first name in the phone book! Insurance generally covers second opinions for major surgery.
Educate yourself about the surgery in general: what can go wrong, and why? what are the different methods?
In choosing a surgeon, standard advice is to find someone who has done this particular surgery a lot and does it regularly. That’s good advice, but incomplete. Our first surgeon had lots of experience and he performs knee replacements regularly. But based on results and what we’ve learned since, this fellow has not kept up with new methods: MRI’s, femoral nerve blocks, post-surgical drains, etc.
Of course nothing is better just because it is new. Some things provide an advantage even the layperson can evaluate, such as the use of MRI’s to see exactly what the joint and surrounding bone look like, so that the operation can be planned using that information. There’s no real downside for the patient in providing better information to the person doing the cutting and sawing. As for the high-tech implantable prostheses used in TKR, there’s always something new coming out, which may or may not be better. You can at least ask a surgeon how long he has been using the device he intends to implant into your body, what the failure rate is, and when and why it fails. Does it fail to be stabilized by bone growth, or do components or surfaces wear out? Does it loosen in 2 – 5 years, for whatever reason? Do particles get ground off and act like grit in a bearing?
Read up on the subject and you’ll get an idea of what to ask. Take notes on your reading and your concerns, and bring them with you; then take notes on what the doctor says. Have someone else come along to help by writing things down, reminding you of questions, and in general giving you moral support. The doctor is the expert, but your body is what’s at risk; don’t be timid about asking. In my mind, a doctor who won’t answer my questions fully, as fully as I want, doesn’t get my business.
Also ask what to expect after the surgery. Surgeon #1 kept stringing us along, telling us that things would get much better. Now we hear from others that isn’t really true, that you “know” right away. And indeed the bad job felt loose from Day 1 and never changed; the recent revision felt solid from Day 1. Certainly, telling us for 2 years that there would still be improvement, was unrealistic (charitable interpretation) and dishonest (blunt interpretation).
More information on Total Knee Replacement
There’s an encyclopedia-style summary of the procedure, risks, failures, etc. here that looked good to me, and another page on this site deals with TKR revisions (re-doing the TKR).
Wikipedia also has good information.
How to reduce the chances that you’ll need knee replacement surgery
It’s no fun, really. And you’ll get stopped by airport security for a special check, every time.

Photo from Wikimedia Commons.
Here’s the advice from the National Institutes of Health––
How Can People Prevent Knee Problems?
Some knee problems, such as those resulting from an accident, cannot be foreseen or prevented. However, people can prevent many knee problems by following these suggestions:
Before exercising or participating in sports, warm up by walking or riding a stationary bicycle, then do stretches. Stretching the muscles in the front of the thigh (quadriceps) and back of the thigh (hamstrings) reduces tension on the tendons and relieves pressure on the knee during activity.
Strengthen the leg muscles by doing specific exercises (for example, by walking up stairs or hills or by riding a stationary bicycle). A supervised workout with weights is another way to strengthen the leg muscles that support the knee.
Avoid sudden changes in the intensity of exercise. Increase the force or duration of activity gradually.
Wear shoes that fit properly and are in good condition. This will help maintain balance and leg alignment when walking or running. Flat feet or overpronated feet (feet that roll inward) can cause knee problems. People can often reduce some of these problems by wearing special shoe inserts (orthotics).
Maintain a healthy weight to reduce stress on the knee. Obesity increases the risk of osteoarthritis of the knee.
What Types of Exercise Are Best for People With Knee Problems?
Ideally, everyone should get three types of exercise regularly:
Range-of-motion exercises to help maintain normal joint movement and relieve stiffness.
Strengthening exercises to help keep or increase muscle strength. Keeping muscles strong with exercises – such as walking up stairs, doing leg lifts or dips, or riding a stationary bicycle – helps support and protect the knee.
Aerobic or endurance exercises to improve function of the heart and circulation and to help control weight. Weight control can be important to people who have arthritis because extra weight puts pressure on many joints. Some studies show that aerobic exercise can reduce inflammation in some joints.
If you already have knee problems, your doctor or physical therapist can help with a plan of exercise that will help the knee(s) without increasing the risk of injury or further damage. As a general rule, you should choose gentle exercises such as swimming, aquatic exercise, or walking rather than jarring exercises such as jogging or high-impact aerobics.
So there it is, same old thing: exercise and lose weight. If you really really do not want a titanium and plastic knee, losing weight is probably the best thing you can do. “Data from the first National Health and Nutrition Examination Survey (HANES I) indicated that obese women had nearly 4 times the risk of knee osteoarthritis as compared with non-obese women; for obese men, the risk was nearly 5 times greater.” Moreover, if you already have knee pain, losing even ten pounds can significantly reduce both pain and the ongoing deterioration of the knee. Being only 10 pounds overweight increases the force on the knee by 30-60 pounds with each step. You don’t need to reach your ideal weight; any reduction will help. And maybe that will be encouragement enough to keep going, slowly, losing weight and feeling better. (Thorough discussion of weight loss and osteoarthritis, here.)

Great article! Thanks so much for taking the time to write it. Very informative and respectful of one’s body. Please keep it updated as you progress post-surgery. Some TKR patients get discouraged as to how long they must rehab after surgery, w/ some taking as much as a year, I hear.
I had a toal knee replacement in 2007 and was just told yesterday that I need a redo. Thanks for your info, now I know that my problem is real and all the trips to the Doctor are worth it. Finally the knee will feel better and I will be able to get on with my life.
Judyann
Where did you get your ‘re do I have to have one and wait times are like a year
Please,all women with 1st and 2nd knee replacements, and still in pain—-to have their HIPS x-rayed!!!!!
Lyle,
Yes, I can well believe that TKR rehab could take a year. And we all want instant fixes from medicine. But I would encourage people to regard it more as a long process that starts off, after surgery, with a status that is probably a bit better than before the surgery (there is post-surgical pain, for example, but it in my husband’s case was less than the pre-surgery pain, and no longer keeps him awake at night) and that will continue to get better and better with exercise and care. It’s like acquiring a new skill—playing some sport, or a musical instrument, or learning bridge or poker or computer skills—you accept that improvement will come over time from practice and learning. Here, your body has to recover from a major assault, the surgery, you may learn to need to walk differently after years of favoring one leg, and you have years of muscle disuse to recover from. The physical therapist Dan saw evaluated all his muscles, including “core” & “glutes”, and taught him exercises to strengthen all of them, not just the muscles in the leg. He is feeling stronger all over and working on walking differently and different posture.
No instant fix, but with the same kind of application that we give to learning some new significant skill, the change in one’s life will be unbelievable.
Dan is just past the 3-month mark. He is not going to PT but still does the exercises. Last week we walked nearly a mile, going on foot to run errands and have lunch after leaving the car to be worked on. We took our time, for his sake and mine (fibromyalgia) but it was certainly something he has not been able to do for perhaps ten years. And afterwards his soreness was mostly in other muscles, not around his knee.
This sort of progress makes it all worth while. And a month after the surgery we were tide-pooling, for the first time in many years; had to limit the length of time, but still, the surgery made it possible. And every week it is better.
So to those reading this who are contemplating joint replacement surgery, or in the early stages of recovery, take heart! Keep up the exercise and keep a good attitude and the payoff will be worth it!
Thank you for your article. You have given me hope and I hope that your husband’s knee now has full recovery. I had a TKR in 1913 for osteoarthritis and it was fine to begin with then the PCL ruptured 6 months after surgery and was left with a very unstable knee. I had Revision Surgery 12 months ago and to my amazement and grief have been told that it needs to be done again because the knee is still unstable and the present prosthesis is just not working and apparently not doing the job making the ligaments around the joint very badly damaged and stretched. My original surgeon kept saying these things take time but after 12 months of constant pain, two falls involving fractures due to the knee buckling we decided to go and see the surgeon we had seen as a second opinion. We trust him, he is easy to talk with and keen to help me get a better way of life. Added to all that is a right shoulder that also needs replacing – the left one was done in 2012. I have had enough surgery. severe anemia for which no reason can be found to date and the future is very uncertain. But thanks for your No Sleeping Blog.
Thank you for your story you have given me hope. Now I need to fine a surgeon who will take a second look at my knee it has been 5 years and I have no relief. My doctor keep telling me he didn’t do anything wrong but I am in pain everyday even with pain meds nothing works when I walk I have to be careful because it buckle so bad. The pain is very very bad I cry myself to sleep at night!!!! For the last five years I have been very disappointed and my doctor says he did nothing wrong even the second and third doctor say the knee looks good but know one can tell me why I am in so much pain.
I’m so sorry to hear this. If your implant is as crooked as my husband’s was, an x-ray should show that, I think. It was a digital x-ray that he got, and it was very clear. Have any of these doctors given you a good look at your x-ray? Needs to be from side to side and front to back, both.
But I also know that some people have pain after a TKR for other reasons, even for reasons no one can see. Like maybe nerve damage? Or suffering pain with the bad knee for a long time prior to surgery and then the brain “can’t turn it off”. If there is no sign that the implant is crooked and the other doctors have nothing to suggest, you might change direction and seek help in dealing with the pain. Not drugs, they are not a good choice for chronic pain, but other treatments.
This article
http://bit.ly/PainOverview
is a good discussion of chronic pain and some treatments. It can be a lot more complicated than we think. Pain from a physical cause can remain or even get worse after the cause is gone, with the brain continuing to feel it. On the other hand, there are things we can do with our mind to make the pain recede: there may be times in the day when you are really absorbed in doing something or talking to someone and the pain is much lessened for a little time. So training the brain can help us to live with pain and not have it be so dominating in our lives. At my age, over 70, with arthritis and fibromyalgia, I know the truth of this. It is not denying the reality of our pain, just learning ways to have it not be in the forefront of our mind all the time.
I hope you are able to work toward improvement one way or another. My best wishes for feeling better!
Yes, i was wondering if you would be so kind to reveal the name of the surgeon that perfromed the tkr? i would gladly appreciate it.
Correction!! If you would be so kind to give me the name of the surgeon who performed the tkr revision! sorry about that. thanks.
Great article. I had my right knee replaced by a well qualified surgeon in May of 2005. Recovery was difficult as was PT. I currently (Fall 2009) have some limited motion and some pain, but not nearly like I had before the TKR My activities are somewhat limited, but in comparison to before the surgery, much, much better. I have had concerns about symptoms, but after researching experiences, I find that I am doing well. I just need to adhere to the advice of professionals and fellow patients.
Thanks for your comment, Gary. Recovery is slow—I imagine that has something to do with the age that most of us are, when we have to undergo joint replacement, as well as the drastic nature of the surgery. Dan’s knee is still somewhat swollen, after nearly 4 months, but as he continues the exercises his strength and activities increase, and his surgeon was very pleased at his last (2-month) checkup. Having so much pain in the knee for years forces a person to restrict activities, and all the other muscles including the “core” muscles weaken too and have to be worked on. At least some of the exercise can be enjoyable things that he hasn’t been able to do in some years, like walking over rocks to go tide-pooling. He did have to limit the time, and had some increased pain afterwards, but things keep getting better. Best wishes to you for continuing improvement!
Jake,
Here’s the info on the surgeon:
Dr. Shawn M. Brubaker, DO
Shasta Orthopedics
1238 West Street
Redding, CA 96001
Phone: 530-246-2467
his specialty is hips and knees, and within that he has a lot of experience in “revisions” (re-doing other peoples’ surgeries)
Good luck to you!
nosleepingdogs
I’m so glad you wrote this article. I am 1 months post total knee replacement. My surgeon was great, however because this was a workers’ comp injury, some short cuts were made by OWCP. I had 6 days of in-home rehab. Workers’ Comp would not allow any more. Needless to say, I never reached 90 degrees. I have an extreme case of loss of motion (the Workers’ Comp Second Opinion Doctor wrote the lack of care was criminal. I’ve had three Orthopedists (knee specialty) examine my knee, none recommended surgery. Instead they recommended a lawyer. am still looking for that special orthopedist who will do the revision and ensure I will get proper care.
Great write ups -Just had my Right TKR Dec 10th would like to here from anyone regarding issues and recovery.
Right knee went bad had 2 orthaesopic now TKR (all within 3 years) recovery is painful scar tissue think about getting a stationary bike any thoughts.
Thanks
lift weights!!!! biking is real good, buts weights are essential, and yoga or other stretching program.
I just wanted to thank you for your blog and including the name of Dr. Brubaker. I just visited him a week ago. I had to drive 11 hours for an appointment and consultation on my failing painful knee replacement and I think it was definitely worth it. The post operative patients in his office seemed genuinely very happy with their surgeries and I talked to several. I hope my experience with him will be as good as I what I hear from others.
thanks again
I can’t tell you the number of times I reread your excellent article and view the surgical pictures (you’re right, not for the squimish). I’ve had several doctors offer to do a revision, but after reviewing your article, most can’t answer the questions on new techology and whether they use computer generated modeling. I think you have saved me from more aggravation. Still looking for the one who is up on changes and technology, hard to find in a state catering to the geriatric crowd. I refer lots of people to your article. Thank you.
Dave- You can reach me by email for info regarding computer navigated revisions. If the surgeons you’ve talked to can’t answer, they are not the best guys to do the job. Not saying they have to use it, but if they don’t understand it, they are NOT current in their practices.
I HAD TOTAL HIP AND KNEE REPLACEMENTS OVER A PERIOD OF TWELVE YEARS AGO- UFORUATELY MY RIGHT KNEE AND RIGHT HIP HAS BECOME EXTREMELY PAINFULL AND I AM ON DRUGS TO KILL THE PAIN – WHICH I MUST SAY DO NOT WORK VERY WELL- AS I AM ABOUT 79 YEARS OF AGE NOW I FEAR GOING UNDER THE KNIFE AGAIN AND FEEL I AM TO OLD TO GO THROUGH THIS TRUAMA AGAIN
Sandy,
I’m really sorry to hear what you’re going through. It is a tough decision to make. I was on chronic pain medications, mostly methadone, for close to ten years (not very helpful with the pain, just as you say) , and know more than I would like to about their ill effects on mind and body, so that is something to consider. Also as we get older the pain meds make it more likely that we may have balance or attention problems and take a serious fall.
Trying to put myself in your place considering this decision, a lot would depend on my situation regarding recovery—having help and support during those weeks or months would be essential. And of course you would want to have a doctor who was very experienced in revision surgery and geriatric surgery. If you don’t have other serious health problems that would make surgery more risky, maybe you should talk to a doctor with the relevant experience and discuss exactly what the problem is with the implants—is the pain & incapacity going to get worse? At some point this may outweigh your concerns about the trauma. Good luck with this; I wish I had something to suggest other than these kind of common-sense suggestions.
I had my knee replaced by Rebound in the Portland, OR metro area (http://www.reboundmd.com/index.php) 5 years ago. Still OK. According to info, they are doing some even more advanced techniques with Legacy in Salmon Creek, WA (Near Vancouver). Worthwhile contacting. They are team physicians for Portland Trail Blazers and WinterHawks.
In my original post, I talked mostly about the surgery per se. Another aspect to give thought to is the after-care at the hospital. A neighbor recently had TKR on both knees, and while he was very satisfied with the surgeon’s work, his experience in the hospital was not so good.
After surgery there’s a drain in the incision and a plastic collection bag to collect the blood and other fluid and prevent undue swelling. This bag is changed regularly and staff is supposed to record the volume of fluid lost and, I think, estimate by color what percentage is blood. Evidently nobody paid attention to this, and our neighbor lost 3 pints of blood and was too weak to get up for the mandatory exercise. It wasn’t until he complained (“I feel like I’m dying”), 2 days after surgery, that the problem was noted and he was given blood transfusions. He also got an infection which fortunately was not too serious but easily could have been. I’ve read pre-surgery advice that tells patients to demand that any staff examining their incision wash, right then and there in the room, regardless of assurances that “I’ve already washed my hands”.
In my husband’s case, the morphine pump providing pain relief the night following surgery quit working and the night-duty nurses were completely unhelpful. If I’d been there I could have phoned the surgeon, but I’d been there all day and then gone home to care for our dogs thinking all was well. It was an hour drive each way and I was tired—no excuse, I should have gone back. It’s very important for a patient to have someone on hand to track on things, ask questions, and intervene, and the night and day after a surgery are obviously critical times.
Another person in our area went to a place (also 3 hours away in Redding CA, like my husband’s revision surgeon) that specializes in TKR. Practice makes perfect, or can, in the surgery biz, but in this case the clinic operates like a factory, and once the patient has passed through the surgery they have no further interest in him or her. “Here’s some pain pills, go home, & if you have problems, go to your local emergency room.” So the quality of the surgery was good but problems afterwards were not dealt with well. This patient said she’d never make that mistake again. It’s important to find out exactly what will happen after the surgery, for both routine and non-routine care, especially if you are travelling away from home in order to have it done.
One final note—discuss beforehand what food your loved one might want while in the hospital, check out where to find it, and as soon as the doctor okays it, provide some tasty meals! Hospital food service people try hard, but everything seems to be bland and overcooked.
Well written! The only thing I would add is to check out the hospital and ask these questions:
1) do they have a unit dedicated to care of total joint patients? Chances are, if they do not, you may get good nurses, but not good orthopedic nurses. In TJR, there is a BIG difference.
2) Do they use total joint “pathways” and order sets to roadmap care?
3) Do they offer a pre-op TJR class which includes ‘pre’ habilitation? A few weeks of exercises before surgery maximizes outcomes, and understanding EVERYTHING before its done is critical.
4) What are their complication rates (infection and DVT specifically…) Most good TJR centers have virtually no complications. If they do not trend their complications, they probably have not done much to prevent them either.
5) Does the hospital own a computer guided navigation system for TJR in the OR?
I am the director of Orthopaedics at a hospital in Phoenix AZ and had a total joint replacement last tuesday. I left the hospital on Friday using a cane, and have only required tylenol for pain since day 3 post-op. I have already met most of my rehab goals for flexion/extension and strength only 6 six days after surgery. Although I am still using the cane, it’s mostly to avoid a fall that could reinjure the joint so soon after surgery.
My best advice…ask wise questions and don’t settle for half answers. If the doctor or hospital can’t answer your questions, call other places who have established TJR programs to help you find those answers so that you head into this process with a positive outlook for the outcome.
Denise,
Excellent suggestions, thank you for your expert input. It is especially valuable from someone who has been on both sides as it were, knowing the inside workings and then experiencing it as a patient.
I’m glad to hear that your recovery is going so well.
I will need revision knee surgery,after 4 years, due to scar tissue. I’ve tried PT, hasn’t helped. 78 years old, not physically fit. How do I know scar tissue won’t build after the second surgery, or is there anything to do that would help?
that is a good question. I am 56 years old I believe I may need a revision on my left knee had a tkr in 2016 may still in pain, swollen all the way up to my hip, then my doctor says I may have the wrong size knee. someone out there that can help. I live in florida and just don’t know what my next step should be
It looks painful…I am going to lose weight ASAP. Thanks for this post, it scares me, and pushes me to lose weight.
gcol,
Yes, what a good motivator! and important for people who have actually had TKR, also.
Here’s a paragraph from the Johns Hopkins University Arthritis Center:
Joint Pain is Strongly Associated with Body Weight
Being only 10 pounds overweight increases the force on the knee by 30-60 pounds with each step.
Osteoarthritis is the most common joint disorder with symptoms in the hands, knees, hips, back, and neck. It is unclear exactly how excess weight influences OA. Clearly, being overweight increases the load placed on the joints such as the knee, which increases stress and could possibly hasten the breakdown of cartilage.(ref. 1) For example, it is estimated that a force of nearly three to six times one’s body weight is exerted across the knee while walking; an increase in body weight increases the force by this amount.(ref. 2) However, overweight has also been associated with higher rates of hand OA in some studies (refs. 3 and 4) suggesting the involvement of a circulating systemic factor as well.(ref. 5)
Find the original here, http://www.hopkins-arthritis.org/patient-corner/disease-management/osteoandweight.html
Before reading this I thought only in terms of extra weight increasing the mechanical load on joints, but it appears that there may be other processes at work too. Being overweight causes metabolic changes and may predispose people to inflammatory disorders among other things.
Find a plan you can live with, of changing how you eat and being more active! I have been forced to do this myself not by arthritis–though I have some of that–but by being told I am “pre-diabetic”. So far walking (the dog likes this part), taking smaller servings of food, and not eating sweets or drinking anything but water, are the things I have chosen. And I am having some success though there’s more to do.
i had tkr about 6 months ago and i have had nothing but trouble since then my knee rattles real bad and when i walk it clicks like a barbie knee does when you bend it i am waiting now on getting a test because the doc thinks i might be allergic to the metal but they are trying to find one but i know the rattiling is not right and the pain should not be this bad i have had it drained 4 times since i had it done it does not make any since
In 10/07 had TKR I got Staff infection, tried to wash it clean and pic line, 02/08 infection back did revision removed joint left out 3 months, another pic and antibiotics, put new joint in 05/08 01/09 infection back, removed joint again another pic line put new joint back in 3 months later six surgeries and 3 knees in two years, due to previous removals this joint extends 5 or so inches into femur and tibia, having pain inside tibia, doctor said shaft is hitting inside bone also knee hurts all time also hip hurts, limited distance can walk or stand, doctor said was only 50% success rate for last surgery, thinking of amputation. But I have faith all things work together for good for those who love God so all who are strugling keep going forward.
God bless you and help with your pain and suffering.
I’m glad you posted this. So sorry for all the trama and stress and pain your husband and , you too, went through.
I was just given the news yesterday that I was not a candidate for knee surgery replacement. Complications, meds, pulmonary embolisms, etc.
I don’t know if I should feel lucky to be able to *not* have the surgery (both knees) at this point !
I don’t know either, what a choice! But after his two surgeries on the one knee, my husband thought he was facing surgery on the other one too, another TKR, but the dr told him surgery would not help much at this point and physical therapy would. He has found a wonderful PT who evaluated his entire posture and joints, and started him on a gradually changing series of exercises to undo the adjustments his body had made over many years of knee pain. The adjustments themselves were putting his body out of balance and straining the joints. The PT stresses gradual progress, if it hurts much back off, and is good at giving lots of encouragement, and he’s been doing the exercises really faithfully. Results: measurable increases in range of motion, feeling better, and less pain in knees and hips. I don’t know if this is an option for you but something to consider. Your dr can give you a prescription for PT so ins or Medicare will help pay. Find a PT who does evaluate your entire body and is congenial to you. His previous knee-only PT never addressed these overall issues.
Good luck, and stay as active as you can.
I had total knee replacement in August 2008. Into my fifth week after surgery I feel off my porch onto a slab of concrete. I went to my surgeon and he said that I was fine. I had therapy for 5 months and I am still unable to bend my knee more than 70%. I wake in the night with my knee cap shooting pain, and also during the day. I have found another surgeon. He did x-rays and said that the knee replacement looks good to him. It could be scar tissue which is giving me the problem. He gave me pain medicine and told me come back, if it didn’t get any better… Perhaps we could talk about another knee replacement surgery, but they are not recommended. I am only 59 years old and I can not bend down to garden, look under a bed and lots of problems getting in and out of the tub… I really don’t know what steps to take… Any ideas?
HAve your Hips x-rayed!!
Seems to me you have a problem with the original surgeon who assured you that you were fine. Maybe the original installation of the replacement was correct and good, but what did the fall do to it? What about scar tissue?
Your second surgeon’s advice to take pain medication and wait and see does not sound good to me. Some people develop a lot of scar tissue after surgery and this can limit range of motion. I suppose then pain can result because you are trying to bend the knee, or put weight on it, but the scar tissue is interfering with proper movement and weight-bearing. If scar tissue is causing you problems, then waiting will not help. My limited knowledge is that you can sometimes increase range of motion of the knee despite scar tissue by means of aggressive physical therapy and for this, the pain meds might be helpful, just so you can bear to do the exercises. Clearly you need an experienced PT to oversee this. Or, there is a procedure called Movement Under Anesthesia, in which while you are anesthetized the surgeon manipulates the scar tissue to kind of break it free. I imagine that PT would be very important after that too. Finally, surgical removal of scar tissue or a revision (replacement TKR) can be performed.
Only your surgeon, or another if you feel the original surgeon is not dealing with the problem, can advise you on this.
But I think that the chances of improvement over time are slim, unless something positive is done. Just taking pain meds and keeping on with your daily routine is unlikely (in my opinion, just as an informed layperson) to help. You might get addicted to the pain meds, though, which is not a good thing.
You did not go through all the pain and anxiety and expense of a TKR in order to be in the situation that you are in. If I were you, I would do some research on this (“scar tissue” TKR, and “stiffness TKR” to start) and then I would confront the original surgeon with this—your knee is not “fine”—to see what he or she says. The sooner you deal with it the better. If you’re not satisfied, if the surgeon fobs you off again with “it’s fine”, time to see someone else. The second surgeon is not a person I would go back to.
It is hard to deal with these complications of such advanced surgery; we patients are not supposed to be the experts, yet the experts differ in opinion, cover for one another, and sometimes are not as competent as they think they are. But I do urge you to do some reading online about these issues, (at medical sites rather than just those where people recount their experiences) and then find a surgeon willing to do something about this.
If you need afterwards to do more PT, you might consider how helpful your PT was the first time around—does not sound as if this person was paying attention to what was going on with you. A good PT has experience in dealing with various complications and does not just put you through the standard exercises regardless. You may well need to ask the PT to evaluate your whole-body posture and walking stance, and work on changes that took place due to pre- and post-op knee pain. I described this more in my answer to the previous comment.
You’re tired and in pain, so all this is the last thing you want, but please try to pursue it. Time will not make it better.
Best wishes for your recovery, and let us know how it goes.
Here’s a more technical summary of the ways of dealing with scar tissue following TKR, from this page:
http://orthopedics.about.com/od/kneereplacement/qt/stiffness.htm
Treatment of Knee Stiffness After Replacement
Treatment of stiffness after knee replacement depends on the time since surgery, and the cause of the stiffness. The usual treatments of stiffness are:
Aggressive Physical Therapy
Physical therapy is a useful treatment for a stiff knee, especially within the first three months after knee replacement. Physical therapy can also be considered after this time, but the results are not as good as early physical therapy. A new type of splint, called a dynamic splint, has also shown some encouraging results when used in conjunction with physical therapy.
Manipulation Under Anesthesia
A manipulation is a procedure where no incisions are made. The patient is given anesthesia, usually through an IV, and while sleeping, your surgeon forcibly moves the knee to break up scar tissue. This procedure is most beneficial in the 6 to 12 weeks after surgery. The primary concern with a manipulation is that there is a possibility the bone can break around the implant if forced too hard. This is most concerning in people with osteoporosis or when the manipulation is performed more than a year after replacement.
Surgical Removal of Scar Tissue
Surgical removal of scar tissue after knee replacement is seldom performed, but may be helpful in some rare circumstances. The results of removing scar tissue have not been particularly good at improving motion, and therefore, usually other treatments are considered first.
Revision Knee Replacement
When the above treatments fail, or if the knee replacement parts are malpositioned, it may be necessary to remove the implanted knee and replace this with a new knee replacement. The bone cuts and the size of the new replacement can be modified to help allow for better knee motion.
Determining the proper treatment of a stiff knee after replacement depends on the cause of the stiffness and the length of time since your replacement. Your doctor can make recommendations for your knee based on your specific situation.
Source:
Bong MR, and Di Cesare PE. “Stiffness After Total Knee Arthroplasty” J. Am. Acad. Ortho. Surg., May/June 2004; 12: 164 – 171.
I have been crazy looking for a site like this. I am s/p right total knee replacement approx. 2 years now. My knee was much better than my old one which I wore out playing competive Tennis. They put me off for a long time and just looking inside and cleaning it up about 6x’s. At age 50, I decided to go ahead with TKR. Last month,I fell which caused blunt force trauma. Pain is bad. I’ve tried all the stretchs, rest, Ice, you name it . Do I just go back to surgeon and see what he can do? Is a second surgery worth it at my age? I am just mad at myself. I took PT very serious and now this. Please help. I neglected to say my L knee lost it’s ACL and I had no surgery after that. On cruthes for 9 monthes…..approx. 1994. thanks, melissa
I’ve been reading everything with so much interest. I have had two TKR.s over the past three years. The first one is awesome. The second one , done 9 mos after the first, is horrendous. I had the femoral block so didn’t notice anything at first, but I sensed it was “different” right away. The same doctor did them and I believed in him so much. Great reputation, wonderful bedside manner, all of his staff are friendly and listen BUT, the second knee was not the same. During the first couple weeks of healing I would mention it was nothing like the first and was told all knees are diferent and they don’t do the same. The pain was different and it never has healed like the other one. I sit here writing this 1 and 1/2 years after the second knee with sharp pains shooting from my knee. It kept me awke through the night.
I have been back, several times. I told him a month ago that when I sit and am getting up I get a sharp , make you yelp. pain and it locks up..His explaination? The tendon is short in that knee. Which causes the tightness and pain.
I saw the xrays with the two knees after the 2nd surgery. It looks like the “screw” is coming out of the bone of the 2nd replacment. When I commented on it , at first, I was told it was the angle of the xray. Made no sense to me but I believed him. I continue to see it when I go back and I get blown off when I ask about it or directed to something else.
I am in as much pain , including my lower back and hip, which I NEVER had beforethe 2nd knee surgery, as I was post surgery. He xrayed my back and sent me for an epidural.
After reading all of this I am just shaking my head at what the possiblities are that this surgery was just flat done wrong.
I am on Oklahoma so I will now begin my search for a surgeon who is experienced in revisions. Although the right leg ended up much shorter than the left ( first one) I am willing to limp a little more if the pain will stop. Although the thought of going through this again is frightening.
Thank you for all your information.
Debi,
Oh this sounds too familiar. I am sorry you’ve had to go through it. Because of the long recovery time for this surgery, I think it is too easy for the surgeons to placate us and string us along. It’s always “going to get better” or “you can’t expect it to be like new”.
It seems like a problematic knee tendon after surgery cd be addressed by physical therapy, though I think many doctors don’t know or appreciate what a good PT can do. And I wonder, if one leg is shorter than the other now, shouldn’t that be resolved with an orthotic or shoe insert? You are bound to have back pain if you are walking with uneven length legs.
Do search hard for someone experienced in revisions, and see what they say about what the x-rays show. My husband’s knee is not all he would wish, but he is able to go for longer and longer walks and is not in constant pain. Much better than the first time around.
best wishes with this!
Nosleepingdogs
I HAD LEFT TKR IN SEPTEMBER OF 2010, DID ALL OF THE P/T FOR THREE MONTHS. AFTER THE 6WK, MY KNEE WAS BENDING AT 106. SURGAN SAID SHOULD BE 110, WENT BACK TO SURAGY FOR MANIPULATIOPN, AFTER MANIPULATION I WENT TO P/T THE NEXT DAY. AFTER P/T I DID NOT BEND KNEE PAST 110 ??? SURGAN TOOK SAMPLE OF BLOOD SENT TO A ORTHOPEDIC ANALYSIS IN CHICAGO. THAT FOUND THAT I HAVE A HIGH REACTIVE TO NICKEL. I WILL HAVE TNR TO REMOVE AND REPLACE WITH A TOTAL TITANUM KNEE. THIS INFORMATION WILL HELP ME TO ASK THE PROPER QUESTION ON THE PRODUCER, THANK YOU ALL AND GOD BLESSING ON YOU ALL
EZELL,
I’m really sorry you are going through this—having this operation once is definitely enough as we well know. But I hope this second time goes perfectly, and you already know what to expect and how important the physical therapy is. Glad some of our experience was helpful to you, and best wishes.
I have had both knees replaced. Both done in 2015 May and November. 1st one was ok I thought still swollen but not much pain so decided to have the other knee done in November. Both of them are titanium. Right after Christmas I started having major pain in both of them. Doctor said it was tenditis in both knees. At this time both knees still have swelling so I am still icing and elevating. Doctor took lots of X-rays on my next visit. X-rays looked perfect he says. I’ve always told him that my knee cap is on the outside of the knee. But of course X-rays are good so he never would even feel of my knee. My last visit 2 weeks ago dr decided I must be allergic to the metal. Even though my knee is the new titaniam knee dr says it still has some nickle in it. I am scheduled to have allergy test done but there is only one dr in my state that does this testing so I can’t get in until November.
In my opinion my knee cap is misaligned but dr says not possible because this knee has a notch it fits in. It is very obvious that the knee cap is not in alignment. I can’t get up form a chair without using both hands and then it still so painful. I can’t do steps without bad pain. I can’t squat to look in lower cabinets. Now it is May 2016. Right knee was A year ago. My left knee was about 7months ago. Dr says come back in three months. I am so frustrated. I live in Kentucky and need a second opinion. Any suggestions? I will be glad to travel.
I’m sorry I’m just rambling on.
I started out to reply about the possibility that the titanium knee still has nickle. I feel that I am allergy to the titaniam knees I have because they feel like I have skint them really bad. They have felt like this since surgery. I thought it would get better but it has not. I could live with that pain if my knee caps were in alignment.
Go to Dr. Cui ( kwee) at the University of Virginia. He saved my Dad’s leg. His original doctor didnt know how to treat the repeated infections , so he wanted to amputate! I told me Dad “hell no “!!! He had the surgery up at UVA 3 yrs ago and has been great ! No antibiotics!! We love Dr.Cui and UVA!!!
i just had my second knee replacement Aug 11th 2011 with almost 2 months post op The pain is not much better than it was before the second op. I am not sure if I will ever be pain free again in my life. I have not had more than 4 hours sleep in I dont know how manny months. The drugs keep me in a state where I forget all the time.
I live in the Uk but I had a TKR last year- August 2010. I was in hospital for 5 days.A couple of months later, I fell from a sitting position on to a laminated floor onto both knees. Over the following 7 months, my knee got stiffer and stiffer and I was referred back to my consultant. After several tests and a biopsy, I went back into hospital for 1st stage revision of TKR- they took out my knee joint and put a spacer full of antibiotics,I was in hospital for 18 days. I wear a brace on my leg 24 hours a day and walk with 2 crutches. I was on antibiotics, IV five times a day for 5 weeks, then orally for 3 weeks. Whilst on antibiotics i was having weekly blood tests. I go back to hospital on the 28th of this month for part 2 of the revision, when I’ll have a new joint put in. hopefully this will be the last operation on this knee for many years. My consultant is amazing.
I had TKR in Sep 2007 on my right knee and I am still experiencing problems. The Doctor who performed my surgery alsoplaced a screw into my MCL to secure it to the bone since it was stretched. 4 months after my surgery the Doctor retired. I started seeing another Doctor and he notice that the screw was working it self out. The knee constantly buckles and I am in constant pain. I use over the count meds as to save on perscriptions. I have been told that I need a revision but I find Doctors reluctant to fixs someone elses mistake as the article states. My left knee is starting to give me problems it is always sore and I have experience swelling at times. I still use my cane as needed to get aronund. I had one doctor tell me that I may be on meds the rest of my life due to the knee. I use a stationary bike and sometimes an eliptical machine to exercise as to control my weight, often after exercising my knees are sore for 3 to 4 days before I exercise again I just want to be able to walk without pain. Thanks for sharing your story. I know that their are others that have and are experiencing the same problems as myself.
What a great site was told today that a redo was needed on my TKR which was done 2 years ago after 1 year of constant pain they did a patela resurface which was meant to aleaviate the pain but no it got worse and my knee often gives way when walking and I get a lot of pain up my thigh. Dr’s constantly telling me its not my knee but my hip or else my brain confused as to where the pain was.. I kept on insisting it was my knee and now with a new consultant he agrees it is my knee and that he will do a redo for me hoping it goes well this time really worried but fingers crossed
hi nice to see the article..After reading this article really i got lot of information on TKR thanx alot.and god grace finally u got good doctor to treat ur husband.ur so lucky…I met with an accident in the age of 12 years that time my right leg thigh joint was fractured and treated with a rod.and after one year it’s been removed and then after we have realized that my knee joint is started bending then again we wnet to orthopedic then they did one operation and they put a rod at my knee joint to stop bending and then after one years its been removed..due to the growing age my right leg is got shorten by 1 inch.So for that Shortenning iam using a extra heel in my shoe…now iam 32 year old.now these days frequently iam getting back pain some times in hips and some times in mid spine area.so i consulted a ortho again so they asked me to take several positioned x-rays after that doctor told me ur knee is in danger condition so u may need to go for TKR but same time he told me its not compulsory rightnow for the timebeing u just prolong it as much as u can miantian after taht we will think of it technology is growing up so wait for some time.i really got scared and in this age if i go for knee replacement so how it is gng to be?iam residing in india so can u give any advices to me to prolong the TKR for as much as i can..again thanx alot for the information which u shared with lot of people..
Anyone experience “snapping and clicking” sensations , and sounds when walking? I am 4 weeks out of a TKR revsion replacing a partial from 4 years ago which failed. Also, mornings are impossible, knee is bound tight as a drum and painful. PT says i am doing ok?? At 115 degree flexion. Pain is similar to a non stop toothache!
I am still experiencing that snapping and cracking and it has been over 4 years now. Knee is very painful mainly due to MCL, but TKR feels as if it has slipped out of place.
This has been good, thank you. My husband had a knee replacement last Novemeber and from the begining, I knew it wasnt right. He has been in pain, walks around like Douglas Barder, and is knock kneed, making him look like the footballer, Pelle. I have been back to GP with him twice, asked for a second opinion, which the first time was not offered. The GP, as nice as he was said that we should trust our surgion, Ha, how can you trust someone who brushes your problems under the carpet. He actually supervised when the registerar carried out the operation. We have gone down the complaints path, and having since been to see another surgion, have been told that the cuts were out of alignment. John will have to have the replacement done again, and I am so angry, not anly because of the risks involved, but the pain that will have to be endured twice over.
The name of this surgion is J Wootton at Wrexham hospital in North Wales, a little man with a chip on his shoulder who isnt able to make eye contact.
I had a gut feeling about this man when I met him, and I was right. He didnt reply to a letter that I sent him last July, asking for reasurance, and asking him questions. Pip squeek. He has what I call, little man syndrome.
If anyone can offer any thoughts of comfort and reasurance for us I would be greatful. I`m worried becasue of all the risks involved, that being heart attack, stroke, infection, clots, nerve damage, etc, I know they have to tell you these things, but it could have been avoinded if this excuse for a sugion did his job properly. Wendy.
OMG – I will be 70 in January and am needing knee replacements – probably a direct result of pacing wards as a registered nurse for over 50 years!
My Uncle had them done a couple of years ago and has said that the glue is leaking and causing an infection. What glue? Cannot see anything about this on internet!
I am diabetic and have high blood pressure and after reading all the comments feel very wary of having surgery. I don’t heal well. A foot operation had to be redone and still is painful after almost 6 years!
I was told at my last hospital appointment that I would only be in overnight – this seems to be not the case – even though I have nursed all my life I do not wish to stay in any longer!
Perhaps the only thing is for me to not have the operations and carry on coping?
I just had my doctor’s apt this morning to go over the possibility of re-doing my total knee replacement. My situation is almost identical to the one you described….the doctor in the first surgery did a terrible job and I knew from the first day that it was wrong and my knee was not on straight – turns out my knee is off to the side at 9*! I’ve been in pain, have no stability and it has completely damaged my gait and alignment, so I am going in for the re-do……this time with a doctor who knows what he is doing!
Mary, I would love to hear an update on your January 31, 2013 entry here about knee not straight. I have the exact symptoms and am going in for an appointment with my Orthopedic surgeon. I feel the femer turns outward (slew foot) about three degrees. It causes a wobble at the knee on every step. The knee snaps and crackles. It hurts and I feel unstable on it. What did you do? Fred
Thank you for writing this i had a full knee placement in sept. Of 2011 it pops loud it makes me cry i cant walk very far i cant stand to work it feel like it is rubbing on top of the parts my dr told me that everything is just fine i have told him no it hurts so now i have no dr no ins so now i am in very bad pain day in day out anything u can tell me i would like to hear thanks
Im 62, had 2 TKR on right knee in he past year. I will probably die from the pain. They both failed leaving me in bed 22 hours a day, in severe pain. And the surgeons and hospitals never talk about the deadly consequence of a failed TKR.
My first replacement lasted 12 yrs
It was bad for 32 yrs, 16 to 52. Fn football
I started having problems today.
Lose, unstable. My doc toll me it would last 10 to 15 yrs depending on whether I had a sedentary or on the leg professional .
At the time I was sedentary. I was bumped to a standing position. From a school counselor to a Special needs teacher.
Then to working at 10 middle schools. (Intermediate Centers moving my office 22 times a year). The second knee wore out from walking on 1 leg.
Insurance runs out June. 25 after my divorce.
Seeing same surgeon fast Freddy Ferlic. FYI
The less time the turnicate cuts the blood flow off to your leg the faster the recovery.
Thanks for your story of the knee replacement.I’m 41 and also had 2replacement and it’s still is right.I need a 3 replacement but don’t NO whom to turn to please help.
I am facing a replacement after 15 years
Original replacement was great
Surgeon tells me revision is serious because of increased risk of infection – up to 20 percent
And increased pain and recovery post op – 20 times more painful and difficult
Anyone have a similar experience
Hi there i just read the artickle of dan, total knee replacement and i also had gone threw the same operation and all the experience and difficults he had gone threw it happen to me too now and i only had once a total knee replacement and i do not know what to do because the doctor that operate on me also said that i must practise which i do but i still have some irritating pain, is there someone who can help me please. Kind Regards
Hi had a total knee replacement in 2011 and i still have some difficulties, the common difficult is the pain that i have, and i do the same work i had done before the operation because i can’t bent,i can’t stand too long and also can’t walk long distance then my leg just colleps, can someone please help me. Kind regards
People, I had a otal knee replacement 5 years ago & it was really.In pain all the time. By the way the Doctor that did the operation has lost his licence to practice medicine & is in Jail at the present time. I live in Maine, I’m looking for a Doctor in Boston or Portland Maine. Any advice would be greatly appreciated. Thank You.
,Not only did i have a bad total Knee replace ment ,
I complained To my Dr for years and wrny in a.and saw him he said nothing was wrong my pain leVal was so past a ten then I started to see other Drs. .No one does like to another surgeons casr , 5years later another surgeon sees my mri and where I complain after seeing five Dr s one tooK my case. The wrong sixr of hard ware had been used and My leg was coming out of the cup..I just had a total knee re ision and still in pt. Please do your research and ask guest questions.I live in utah and
m looking for a perso.nal injury lawyer if you know one please contact me. I write this thru tears so please forgive me.
This is the most informative site I have come across. I have read the ,comments and feel your pain ,tears and flustration and the Dr s who won’t admit a mistake , and our words fall on deaf ears.I used to live in the UK and this is the best site I have come across tha.nk you for all the hard work putting this site together and for all of your heart felt comments.drs should have to read the damage they have done and pain they caused
I had bilateral TKR 5 mos. ago and although my new knees are stable, I have several different kinds of pain. I have a difficult time doing the quad strengthening exercises without days worth of pain over both patellas. The skin burns, deep itching, jabbing pains and extreme surface pain. I feel like clawing the patella out and wish I had never done the surgery. I also have a lot of tendonitis behind both legs that makes exercising painful. I’m only 55 and was active before all of this. I’m on lyrica and Mobil and am now looking at nerve blocks and cryoablation. Does anyone have good results with this procedure?
Did they happen to diagnose you with Complex Regional Pain Syndrome? Or has anyone talked about neuromas?
No, it’s the geniculate nerve that has been set off. It only transmits pain. I’m having cryoablation done to freeze the nerve, 1knee at a time. It’ll last between 3 mos to 2 yrs. the pain spec. Did a nerve block to see if that was the nerve causing the pain and I was able to bend my knee without pain for about 8 hrs. He said that they don’t know why this happens- occurs with other knee surgeries not just replacements, and I’m unlucky enough to have it in both knees!!
Hello, my dad has had several tkr surgeries. Actually, 4 replacements each ending with an infection! My dad has gone through at least 13 procedures over these replacements. We know he’s not allergic to the device. I really think the doctor never diagnosed the first infection correctly. I’m thinking if you’re trying to treat infection A , but it’s actually infection Z, you never get better. Now they want to amputate, not because of poor circulation or anything else, just because infections are so hard to treat. I’m looking for a different doctor for my dad!
Thank you so much for writing about your experience. In 2009 at the age of 47, I thought it would be a great idea to start riding my bike to work to get into shape. I lived in an upstairs apartment, so I had to carry my bike down each time. On the 2nd day one of the pedals got caught on the banister and both the bike and myself tumbled. My knee hurt but not enough to stop me from getting to work. By the end of the day I could not walk. I went to urgent care, where they put a brace on and told me to see an Orthopedic Dr., but of course I put that because my leg felt like it was getting better. In August of the same year my leg locked up, so I finally went to the doctor. I saw him on Wednesday & on Friday I was in the operating room the only test he did was an x-ray. I had ruptured the meniscus, torn all the ligaments & tendons, dislocated the patella, & had severe osteoarthritis. The doctor said he fixed it the best he could. February 10, 2010 I had a TKR on the same knee. Between the 1st & 2nd surgery I had begun seeing a pain management doctor who did not prescribe enough medication for the pain that I was in. Due to his lack of understanding I was unable to use the CPM, do PT, or any exercises as often as I needed, therefore, I had to have a manipulation (which was the worst pain I have felt in my life). We finally got the proper medication, I was exercising, walking 2 miles everyday, & was actually able to get a job for a few months. In July of 2012 I fell down some more stairs & ruptured the Quadriceps on the same leg. I went back to the same Orthopedic surgeon, he felt my leg, did an x-ray, & into the operating room I went. I was in a straight brace for 4 weeks and then, at a very slow pace was allowed to start bending my leg. I am still in excruciating pain and taking way too many medications. About a month ago my leg starting feeling like it was going out from underneath me, so I went back to the same doctor who told me, “I am up against a brick wall & there’s nothing I can do for you.” What kind of doctor says that to a person?
I have now been referred to another Orthopedic Surgeon, he is supposedly the top in his field. He specializes in patients with prior TKR’s. He gave me 3 options:
1. Remove the patella because it has dropped out of position.
2. Replace the knee with a different style.
3. Amputate the bottom half of my leg.
He stated the first 2 options do not look good for me due to nerve damage.
At this moment, I am so angry that with all of the technology we have today, these are my only options.
I do not want to accept that these are my only options. If anyone has any ideas please tell me.
Hello, sorry to hear about all that you’re having to endure. I emailed a Dr. in NY and he told me to search for a high volume complex revision surgeon. This is my advice to you also. I think it’s crazy how doctors are willing to cut your limbs off when they can’t figure out what to do. Keep your leg and strengthen your mind and body. Seek another doctor in a different facility or entire new area if you have to.
I would like to know the name of the Doctor in NY. I AM IN NEED OF A REVISION OF TKR.
Greetings from southwest Colorado! Indeed, I live here to enjoy the beauty and serenity of 13,000 foot peaks, hiking that is..”Until one year to the date”… I fell from a ladder,only to hear that I had a meniscus tear Rt knee. My orthopedic Dr also informed me that I have osteoarthritis. I elected to have the meniscus repaired. after rehab for this basic type surgery, week after weeks and than months, I called my surgeon for help. I had cortisone shots, and then a synvisc injection. No relief what so ever. after the meniscus repair, the osteoarthritis kicked into super turbo high gear. I am now pretty much disabled. I am having TKR on February 1st, 2014. day after the Super Bowl 48 “GO BRONCOS”. After reading all of the post’s, I see a lot of depression from the readers. I believe that when you under go any major operation such as total knee replacement that you need to keep yourself as hard as it seems “focused” on your recovery. Stay anchored to your Desire, I desire to be well, I desire to live my life without pain, when we numb out our natural longings, it affects all of our senses. I want to thank you nosleepingdog for this truly awesome,educational site.
Dano:)
I am now 9 mos. post bilateral knee replacements and have found out after my surgeon sent me to a specialist, that the burning i am experiencing is from neuromas formed from the surgeon cutting through the infrapatellar nerve. If he had cut down the center of the knee instead of going around it, he would have missed the nerve completely. I now have to have microsurgery to move the nerve and bury it in muscle. Also, my ligaments are loose and the tibia and femur can be slid back and forth causing the painful tendonitis i’ve been experiencing since my 1st week in rehab. The fix for this if non-steroidal anti-inflammatories don’t work, is another bilateral knee replacement with a different type of implant. My original surgeon thought he walked on water… at least he sent me to another Dr. for a second opinion!!
Robin, I had the same issues with neuromas and actually has them removed about a year after my left TKR. It made a huge difference. I saw a specialist in Milwaukee WI … I understand there are a lot of docs who specialize in this so if you’re interested in the info let me know.
I meant to say a lot of docs that don’t specialize in neuromas 🙂
Jennifer thank you so much!! It’s good to know that your surgery helped. The specialist referred me to a plastic surgeon he uses for this surgery so I have a consult with him in 2 wks.
Yea i would like this.information i have had meany surgery on.my knee then infection i live in kanasville wis looking fir someone in.Milwaukee and also.if u no of a good medication management Dr it would be great i am.haveing trouble and more trouble thanks u can reach me at bdaiseyfella@gmail.com
Awesome Robin … Best of luck to you!
Now this is what I am talking about. your desire was to get to the bottom-the very bottom of your core, to find what was causing your displacement in your mind. you were asking your soul subconsciously that you desired to find an answer. congratulations Robin. when we desire, “we succeed” I am sure you will recover, and run along the beaches one day..
Dano
I had a knee replacement – after 15 months the pain was worse than before surgery.
I had a redo replacement surgery by another doctor who said there were obvious problems with first surgery. Is the first doctor responsible for at least my high insurance deductible and other cost not covered?
Thank you>
How does your knee feel now after the revision?
Thank you for this blog. That’s all I can say. You most definitely have made this blog into something thats eye opening and important. You clearly know so much about the subject, you’ve covered so many bases. Great stuff from this part of the internet. Again, thank you for this blog.” Subsequently, after spending many hours on the internet at last We’ve uncovered an individual that definitely does know what they are discussing many thanks a great deal
wonderful post
Knee Replacement Surgeon in KukatPally
I had my second surgery on my left knee by Dr. Chevetta at Raleigh Orthopedic in Raleigh. I was back at work in 2 months walking for 5 hrs a day. Some pain but, after about 6 months it is fine. I first surgery replacement on that knee was 16 years old. I am 73 years old and weigh about 190 lbs. I should lose weight but, probably will not.
Latest medical devices for hip replacement: Ovation Tribute hip stem which can be used totally in total hip replacement and hemiarthroplasty procedures.
I also have been known to never dive before I check what lies below. I have had a partial replacement medial right knee against my better judgement. Now I am laterally becoming excruciatingly off the pain chart…oooh, the pain chart when pain is so subjective and personnal. However, if you would share where and who created a happy place for you and yours I would be most appreciative. As a R.N. I find that anything positive is received with great perssonal pride, much as an artist. It would also be noted I am aware no two results are ever the same.
With appreciation and respect,
Martha Andriekus
P.S. Did you know there are sites for journal articles by lay persons? Your article was superior..almost makes me wonder if you secretly have some medidal background. KooDoos (kids tell me that koodoos are the best)
what about the feet removal..is dere any alternative for replacement?????/
Only with what is called a prosthesis, an artificial foot that would be removable (not permanently attached to the leg) like an artificial leg. I don’t know anything more about this.
can the injuried person walk properly after a replacement..n how much would it cause?????
With a knee replacement, which is what this page is about, yes the person can walk but there may always be some pain and stiffness. In the US these operations cost many thousands of dollars, $30,000 or more including time in the hospital.
If you are referring to foot replacement, I think some people walk quite well afterwards but really have no knowledge about this or its cost. Except very expensive. The feet may be made just for that person, or at least the person has many types to choose from. In other countries prosthetic feet and limbs are available that are more simply made and much cheaper though they may not work as well or be as comfortable, still the person can walk.
Due to a work injury, I had bilateral TKR in January of 2012. I was hospitalized for 8 days a that included physical therapy. Once released from the hospital I began outpatient P/T. After one year recovery I complained to my surgeon that I felt like the right knee replacement wasn’t rehabbing properly. Something just didn’t feel right, and there were many things I could do with the left knee that I just could not with the right. He insisted that it would take time, and I just gave it time. During a follow up visit in May of 2013 after continued complaints from me of pain, swelling and what I thought was a misalignment, my surgeon admitted that yes, maybe something is wrong with the right TKR and referred me to another surgeon. The second surgeon was seen in June 2014 and advised me that my original TKR of the right knee was a failure. Slightly misaligned and the only correction would be a total revision. That total revision was done in August of 2013. The original replacement was removed and a new one installed, with titanium rods inserted above and below the new knee replacement. The recovery has been slow, with a continuous limp, and nagging lower back aches I was recommended to a chiropractor. The chiropractor relived me of my back pain, and the limp was corrected. I began to walk a maximum of two miles a day and all was going well. Then out of nowhere, I began to experience lower leg pain from below the knee down to the ankle, with daily swelling. I consulted with my surgeon who advised to cease walking on concrete surfaces and go to a soft track, or treadmill. This did not stop the pain, which is not severe, but continuous. I’ve ceased all unnecessary walking and only use my recumbent bicycle. It seems that any weight on the right leg causes the pain to flare up along with swelling. I have a follow up appointment with my surgeon on December 2, 2014. If anyone has had a revision and can relate to this issue please share your experience. I’m concerning that inserted rod may be loosening, or the bone is not growing properly around the rod.
I got this web site from my buddy who informed me about this site and now this time I am browsing this web site and
reading very informative articles at this place.
Had revision TKR 12/14, rehab was so much easier than original, completed 120 degrees in 3 months. But at 5 months developed horrific knife like pain in the Tibia from the knee all the way to the ankle. Now for 7 months I’ve been barely able to walk. Last month my surgeon had me go 4 weeks off that foot (with a walker, couldn’t do crutches as recent 2 rotater cuff surgeries in 1 shoulder). Would hold as much weight as possible with arms on walker, and spent a lot of time in my recliner. Then 2 spend the 5th week gradually adding weight. He also ran labs for infection to rule it out. But didn’t help any & going back 2 surgeon today. Am totally frustrated. Nothing helps this pain. It’s weight bearing and especially in a turn. If I am up 30 minutes or so, the pain with my feet up continues 4 hours. I’m on Percocet 4 other problems, spinal fusions and bone grafts, 2 shoulder rotator cuff drastic surgeries (from a drunk driver hitting me), ankle surgery since 1974 leaving minimal movement & still pain. Finally 2 internal Neurostimulators implanted with wire down the spine which should control pain, LOL. Sometimes yes, most of the time from the waist down yes, but does not touch the shin pain. Have tried all kinds of topical, no use.
HELP!
Saw Dr. today & now I’m to be in a wheelchair for the next 6 weeks! He said it is the lack of the bone being able to surround.the stem. He says it’s normal to get the pain around 5 months, and now I’ve had this pain 6 months. He said I have to keep weight off it as that is keeping it from healing. Also said to take Vitamin C every day. I can take a few steps when necessary, but wheelchair primarily. So guess that’s it for me for 6 weeks and see him 12/28 and I’ll see what happens. I do have permission to use my recumbent bike as there is no pain with that, and the few steps in and out of the spa. He even said I could go back to pool exercises as there is no pain when in the water plus I do 3 laps in a very large pool. So maybe being active that way will help lose the 13# I’ve gained back being inactive from the pain. Update 12/28.
CS, your pain sounds like mine, but mine is so sharp, like a knife pain, I believe it’s nerve pain. See my posts and what my Dr. is having me do. I don’t know if this is the right approach, but does sound like it may work, fingers crossed. Mine is a revision TKR, so the stem is longer into the tibia. Many on other sites say that their Dr. said it will just go away, but 6 months of severe pain when I have so many meds to combat nerve pain, it doesn’t help the tibia pain at all. Mine starts at the knee and follows the tibia all the way to the ankle. I can lightly touch the tibia and run my finger down to the bottom and it’s painful, but not agonizing like this. I’ve taken 4 falls already, 1st three I was caught or grabbed something. Last night when I stood to go to bed, it was so bad, I went down, crushing stuff on the floor, ornaments, boxes, and landed 1/2 way on the coffee table. Both knees sore, and deep scratches but after 15 minutes I was able to make it to the couch and pull myself up. I can’t afford falls like this with the other knee close to needing replacement, and much of my spine fused and bone grafts, as well as a bad ankle that gives out. So I have to get this controlled before I hurt myself badly..I’ve had over 30 surgeries and am determined to not have any more. This is the 4th surgery on this knee, the 3rd being the 1st TKR. After 5 miserable years, I saw my current surgeon and told him I couldn’t spend my life limping, in pain, and more. When he replaced it, he found the 1st TKR parts were hard cemented in 30 degrees off. No wonder.
I had knee replacement surgery in 2010 I still don’t have full range of motion I can’t bend it all the way I can’t squat at all
Marnita Simpson. I worked like crazy trying to get range of motion, but it was physically impossible due to the surgery. From what they told me, headway needs to be done asap after surgery and this time I got 120 degrees in 2 1/2 months. Tried for more, but couldn’t do it. I’ve been told by therapists to never squat, in the spa it’s a mini-squat….never put your knees further over past your toes. Now since 4 weeks on a walker only touching the toe of the affected knee for severe shin pain, it hadn’t helped, I am now on a course of 6 weeks in a wheelchair and only a few assisted steps when I have to do up/down stairs. Talk about depressed! 6th day and I feel like my life is helpless. Do have permission to use my recumbent bike which does not hurt the pain at all, and the steps up/down for the spa for water exercise. He wants me swimming, but 80 minutes round trip which is harder, but will try. I can do the leg kicking in the spa, as well as many of the other motions.
So, Marnita Simpson, doc after doc has suggested swimming, so if you have access, try it. I do a 45 minute fast exercise class as well as 3 long laps. It helps the knee stay moving. I was told for the revision TKR and 2 shoulder surgeries (rotator cuff) that is termed a “trick shoulder” now that constant exercise of these 2 areas is important.
One of the most concise articles on line that I’ve found.
If I had just one comment to make, please younger people, that heed when your doctors tell you to exercise and lose weight. It is so key to hopefully never have to go through this.
I didn’t and have ankle surgery, 4 surgeries on rt knee, semi-ready for lt knee TKR. 2 shoulder surgeries, 2 neck fusions, 3 lower back surgeons, and then epidurals throughout the spine, then nerve cuttings at many levels of the spine, ending in 2 permanent Neurostimulator implants that help control all the sciatic and other pain caused from the surgeries, which takes me about 4 hours a day just to sit and charge the internal batteries. Plus other surgeries (about 6 major). Other than the shoulder (stupid drunk driver hit me doing 75 mph), and ankle (accident).
The spine, knee, hips, etc. are in such a large chance for damage due to overweight. I was one of those that ignored the doc who said I’d be in a wheelchair in 10 years. Well, not quite….it’s been 23, but if this leg shin will resolve I’ll be walking again.
Meanwhile exercise, from lack of on my shoulder I can only raise 1/2 way now. I know now I have to be serious. Had gastric bypass surgery, working on getting rid of partial regain of pounds.
This is serious stuff people. Pay heed. So many things can go wrong on knees. You want to avoid this if at all possible.
Thank you
I ahd a total knee done in Sept 2015 and have had nothing but problems since that time. I feel as though i switched one set of issues for another. They removed scar tissue 5 months later and it is still not right. It feels as though my knee has twisted, my foot is being pulled so it rolls inwards, I am in constant pain 10 months later with no end in sight. I have lost 25lbs in weight, i am still stretching it out daily swim three times a week and do pool exercises and feel as though I am fighting a losing battle. My muscles feel as though they are pulling my whole leg of , my muscles fatigue quickly and I carry my leg when I walk according to my husband, It burns from the knee down to my ankle, my hip and lateral side of leg are now hurting and my ankle is weak. I am getting depressed and cannot sleep through the nigh due to the discomfort. This was an injury that occurred at work and they are trying to find someone for a second opinion. I am at my wits end and just had my 55 birthday. Please tell me there is hope
I hope a second opinion helps. I went thru 5 yrs going from Dr. to Dr. until finally one said the TKR had to be replaced. I can’t have MRI’s due to so much metal in my body. They found the original was 30 degrees off from top to bottom, no wonder I could barely move it and constant pain. So 12/2014 I had a revision TKR. Marvelous results, 120 degrees in 2.5 months. Had about 2.5 months, so happy and moving great. Then horrible pain hit instantly at 5 mo. The majority of my body suffers from nerve pain, so I instantly knew what it was. It was from the knee to the ankle. Everyone has a different name for nerve pain, burning is one. I cal it a knife pain. That’s what it felt like. It went straight down the Tibia. So the Drs. tried me hopping with a walker. I had 2 major shoulder surgeries (drunk driver hit me and torn the entire rotator cuff and tore off 3 tendons.) So I couldn’t use crutches. Ended up in emergency as everyone thought I was having a stroke. Back pain so intense, radiating in one arm, and into my chest. My face was so clammy. I took aspirin in case and 13,000.00 later, they were sure it was something major so did a lot of CT scans, Drs. thought I wasn’t holding my leg up enough, but emergency said it was Thoracic Strain. Lovely. So then I was left in a wheelchair 24/7 for another 6 months. No difference in the pain. I had found a possible solution on this site and had told the Dr., but they have steps to take, first was to make sure there was no infection in the knee, then being off of it to see if the soft bone (Tibia) where it was disturbed would harden up around the STEM with was longer and wider in the revision. That nerve pain was horrible. I was more and more depressed and forget anything such as normal sleep. On 02/16 they did the surgery that had worked for the girl I read about on here. The first day stepped on it and no sharp knife pain at all. The ankle was extremely sore, which I found when bandages came off in 2 weeks. The had put in a half round metal the entire length of the Tibia to support it. Once in a while it irritates my knee, but most often it’s mid shin and ankle. My first steps up are very uncomfortable/painful. I have to make sure my equilibrium is good and the first 10+ steps are awful and then it lets up quite a bit. Dr. said I’ll ;probably have 2-3 more episodes in the next year that sent me to emergency, only 7,000.00 this time. Swelling from knee to toes so intense, the skin shiny from stretching and I couldn’t walk. Everyone was sure it was a blood clot. Now I know what can happen and have water pills to take to keep it from getting to that point. So they said come back in a year, guess that tells me the healing (and pain) will take that long. At least it’s not the nerve pain. Nerve pain is miserable, unable to get away from it. So many spine surgeries, and bone grafts, had scar tissue wrap around the screws making the nerve pain worse than before. So now I have 2 Neurostimulators (sort of like super Tens units) installed inside, a wire from the top of my spine to the waist to one, and the other down from waist to end of the spine. Super pain relief! But the upper one only helps about 50% and lately the lowest spine quit being helped. So I’m stuck on Percocet and I hate taking pain meds. I feel relief from them, but don’t affect me any other way now. Except no one told me about the anti-depressants and the pain meds & other meds cause dry mouth which destroyed most of my bottom teeth. I have a slew of things to take, but drink lots of water. And then all the meds have taken a toll on my kidneys.
It’s a crazy life, but I’m curious if your description of burning pain isn’t nerve pain. Something to check out.
hi i hope ou find hope. I feel the same way as you..Im going crazy.
I was wondering if the originator of this conversation is still going to Dr. Shawn Brubaker. I live 3 hours from Redding and find that Dr. Brubaker now works at Dignity Health in Redding. Before committing to travelling out of our area, I would like a quick touch-in before I secure an appointment with this doctor. Just an update would be helpful. Thank you.
Hi I was operated fo TKR Jan16/2018.Since that day I’m not able to fold my knee and my leg is a an angle.I never been able to walk a step and my leg is all the time stiff swallen and inflamed . Now the dr are having a discussion of how to fix it. The Dr which operated send me to a specialist yo cut the femore to put the leg strait. This specialist send me back to the original dr to reoperete the knee again which he do not agree. I’ m waiting to se a fourt specialist for his opinion to how strait my leg .
I’m glad I found this website it has certainly given me room for thought.
i’m 78 and have had two replacement joints which were done within 9 yrs of each other.
They have been excellent apart from certain restrictions such as not being able to kneel
But I have lived with that because I was rid of the dreadful pain I suffered for a number of years. Unfortunately I had a nasty fall a year ago with fractures in my spine which has taken
A year to heal and still get thoracic pain if I overdo things. My right knee got quite a clash
But took a few weeks before the pain started. Now the consultant wants to do some
Revision surgery to fix loose screws etc,he assures me it’s not as bad a operation as the
Initial one and would be easier to get over but I’m not so sure as my consultant hasn’t
Explained what I want to know,it would be really helpful if a surgeon would answer some
Of these questions to give us some hope for instance am I too old for this? I was in and out
The consulting room all of 10mins,I don’t feel I have any faith in my consultant or my GP.
What are other people’s thoughts on this attitude especially when dealing with the elderly.
Great Information about Total knee replacement Surgery. Thanks for sharing.
Did you sue the first dr? I’m in the same boat. Not a bit happy.
I’m sorry to hear that you are going through this. We actually talked about suing, something we both never thought we’d consider, but the dr had strung Dan along (You need more exercise! More PT! Come back in 4 months) until, as we found out, the 2 year limit for malpractice suits was expired. It varies by state. Two years is really too short. The surgeon who did the revision actually said he would say in court what he told us, very rare when they do that I think. We saw a surgeon 200 miles away for the revision so he didn’t know the original surgeon.
It was terrible for my husband: years of pain and loss of mobility, undergoing another surgery with its risks and recovery time, and then the fact that each “revision” shortens the bone, so there is a limit to how many can be done, if infection or problem with the implant should develop. Dan had the first crooked one, then a revision, then a removal/replacement (2 surgeries) on account of infection due to cancer treatment, and finally an amputation a few years later due to infection following more chemo. By that point the bone would not sustain another implant. So the consequences in the future can be serious too. Filing a suit brings the issue to the attention of the doctor’s colleagues and insurance company which may help limit future damage to others. I wish you the best, whatever you decide.
Sorry – didn’t see the typo on my email address
Had TKR in 2016 after about a year I kept falling and was put in Rehab for PT. Now 2019 I was told I have a loose part and need surgery. First one was great also straightened my bowing leg. I’m dreading going throght another surgery but I guess I need it. Right?
Are you able to walk safely without falling? do you have pain? Since you say “I was told I have a loose part” I’m not sure if it is actually bothering you or not. For sure, you have to be able to walk safely, and pain can suck the energy out of you.
Is it the implant itself that is loose, not tightly attached to the bone any more? Here’s a short article that summarizes that problem. It rightly points out that “revisions” as they call joint replacements after the first one, are a serious step. http://arthritis.emedtv.com/knee-replacement/loosening-of-the-implant-after-knee-replacement-surgery.html
As my husband found out, *each surgery shortens the bone*. He had the original surgery where the replacement was put in crooked (surgeon error) and was indeed loose and painful and felt like it would buckle; then surgery to correct that; and then, because he developed bone marrow cancer (from Agent Orange in Vietnam) his immune system was really low and he got an infection that went to that knee and hid. Eventually a 3rd surgery in which the joint was removed and a temporary implant that was full of antibiotic put in for 3 months, no weight on that leg, then a 4th surgery putting in a 3rd implant. When years after that he developed another infection in the knee that couldn’t be conquered there was not enough bone left to do a TKR and he had to have an above-the-knee amputation. I haven’t written about this in the blog as it got too hard.
But there are serious consequences to revisions and the surgeons always act as if everything will go as well as possible. TKRs don’t last for decades, even if all goes well, so depending on your age someday you may need a replacement just due to wear and tear. So be sure you need another surgery, get another opinion, and a surgeon that does a lot of these.
And do you feel satisfied with the surgeon involved? How did he or she account for you falling? It is your right to get a second opinion, both on the necessity for the surgery and on what brand of replacement joint is going to be used. Your surgeon should be willing to discuss all this with you. And find out how many of these surgeries this person does per year. The more the better. You don’t want once or twice a month, that is not a good sign. Practice builds skill in surgery as in everything else. If your surgeon gets offended and doesn’t want to talk to you, maybe you should take your business elsewhere.
Best wishes!
Had colonoscopy today my 3’d one. This one was awful I was sedated but did not work nurse even said shse was giving me more because I said it hurt . The second medication did nothing. The other 2 I was out and did not know anything. Why is that? Have to go back in 3 years but want to make sure that does not happen again!!