NOTE: Four years after this post first appeared, it is still drawing comments from people searching for answers about chronic pain relief. I’ve learned a good deal from some of these comments, and in particular I want to remind readers that my experience with methadone is not typical in one respect: by the time I switched from other opioids to methadone, my most severe pain had been dealt with. My pain from fibromyalgia is chronic but not really bad if I manage my activities. A reader posting as Fireside Academy reminded me that we have to evaluate methadone (and other pain meds) “relative to the pain experience without it”: if my pain had stayed at the severe level it was at when I started with opioids, then methadone might have been a positive thing for me.
Almost all medication for chronic conditions is two-edged, so that we have to choose—are the benefits worth the negatives. All opioids present problems, yet other alternatives may be nonexistent. Go in with your eyes open, remember you need to retain control over the medication rather than letting it control you, and be sure you can rely on your pain prescriber to help you through the hard parts. I recommend scrolling down to Fireside Academy’s post (Feb. 19, 2012) to hear from someone for whom methadone is being beneficial.
I’m going to write the article I wish I’d been able to find when I was taking methadone for chronic pain. The degree of detail will probably make it of little interest except to those using methadone or considering it. (This is not a discussion of pain that results from a terminal disease, or from a disease that is temporary but severe, like pancreatitis. In such cases, opioids may be the best or only choice, and you are entitled to relief.)
I began taking morphine, and then methadone, for pain in 1997 because of crippling muscle-spasm-like pain, every day, from a long-untreated back injury. The injury had occurred in 1981; the orthopedists couldn’t see anything on x-rays, intimated that I was a malingerer, and wrote me off. Constant pain and disturbed sleep probably triggered the fibromyalgia that began to develop after a few years; by 1996 I was unable to work even part-time because of the deep fatigue of the fibromyalgia, its all-over body pain, and the back pain. At that point something had to change.
After finding no medical help in my area I found a pain doctor in another state and went to see him. He could see disc damage on an x-ray, and showed it to me. This is not particularly definitive: pain often exists without visible disk or vertebral damage, and visible damage often occurs in people who report no pain. But this doctor could see my pain in my face and how I moved, and that seemed to be the clincher for him regardless of how the x-ray turned out.
He put me on morphine and made an appointment for me to come back for a lumbar nerve block. This would only last 3-6 months but during that time the muscles that had been clenched with pain for 16 years could gradually unclench and be exercised. The nerve block worked exactly as planned, and I exercised consistently and was able to be more active. As far as back pain goes, I haven’t had a day since which was as bad as any hour in the previous years.
But the fibromyalgia pain remained. It’s felt all through the body: the pain threshold is reduced so much that light pressure feels like pain, a pat can be like a slap, and it hurts to lie in bed, sit, walk, lean against a wall. Extra pain is felt for days or weeks in muscles that get used even a little. As a result I wanted to stay on the morphine pills, thinking that it probably helped.
I couldn’t afford to keep traveling to see the out-of-state doctor so I looked around for a local pain doc and this time I found one. He switched me to methadone when the morphine became less effective. The methadone’s effect, too, became less over time.
Lesson #1: opioid effectiveness lessens as the body becomes accustomed to it. Opioids are not, therefore, a very good approach to chronic pain.
I think this second doctor was hoping I’d want another lumbar nerve block, a more profitable therapy than simply seeing somebody every couple of months for a prescription renewal. As it became clear that continuing exercise was keeping my back pain under control, he stopped inquiring after it, and began to treat me rather brusquely. I was still under the impression that the methadone might be lessening the fibromyalgia pain so I wanted to continue it, but I was feeling more pain, not less. The doctor raised the dose somewhat; he (rightly) resisted my efforts to raise it more, but never discussed any other pain relief measures with me. Gradually I became aware that while I was physically dependent upon the methadone, enduring the side effects and the 6 doctor visits a year, I was receiving diminished benefits or maybe no benefit at all.
Addiction and chronic pain
Here a word about “addiction’’ and “physical dependence”. During the time I took methadone, I have seen a total change in how the medical establishment thinks about addiction and pain patients (though not all members of it have made this change). In a nutshell, addiction is now the term for someone who is both psychologically and physically dependent on a drug. Pain patients rarely fit this definition: they rarely get any “high” from morphine, methadone, codeine, oxycodone, etc. and they don’t start taking it because of a psychological need to feel “different”. However, the physical dependence will cause the same withdrawal symptoms for the pain patient as for the addict, and constitutes a severe barrier to anyone trying (as I did) to get off of methadone without the support of a knowledgeable doctor.
Doctor or pusher, patient or customer?
Why was I trying this without help from my pain doctor? Because he refused to help, denied that there were any pharmaceutical aids for getting through withdrawal, and ignored my reports of having gone through painful withdrawal five times and failed every time.
One of the realities about being dependent upon a pain medication is that you are then dependent upon your doctor. Don’t like him? Not sure you are getting the best treatment? Better not change or you may be viewed as a “doctor shopper” and drug seeker. Of course you’re seeking drugs––that is what the medical establishment has offered you––but the hysteria from the war on drugs, another one of those “long wars,” has infected the practice of medicine with fear and prejudice. Why fear? The DEA, or state licensing boards, occasionally pounce upon pain doctors for prescribing opioids to too many people, or in cases of accidental overdoses. Doctors can lose their licenses, be pilloried in the media, even be charged with responsibility for someone’s death.
So the situation can easily become much like that of a drug dealer and his customers: the doctor/dealer (skeptical of your professed pain) has contempt for you, or is on guard watching for signs of scamming but is obliged to treat you and perhaps wants your money, while you come to loathe him but tailor your every word and expression to avoid getting cut off. I hope that most doctors do not fit this description. But the patients, who are locked into a relationship with wildly disparate power on the doctor’s side, must inevitably come to an uneasy awareness that their wellbeing depends on a “controlled substance” which is entirely controlled by the doctor, and which carries a public stigma of association with being a junkie, a weakling, a fraud, or all three. This is not like knowing you depend on your physician for your insulin prescription or your heart medication. A diabetic or heart patient is never suspected of getting medication for personal pleasure, or in order to sell it to schoolchildren.
When I first visited the callous pain doctor, who “treated” me for ten years, I was required to sign a form. He described it as a contract but all the obligations were on my side. I had to agree that I was aware of undesirable effects from opioids including dependency, and that if I lost a prescription or a month’s worth of pills I would not expect the doctor to write a replacement prescription. The importance of this latter provision is not one that can be understood by the patient until later. Once you’ve become dependent upon opioids, and experienced even mild withdrawal because you’ve forgotten a pill or been a few hours late, you realize in a different way what it would mean to lose a prescription and be without the drug for a month. Each month’s prescription form had to be picked up by me personally rather than faxed to the pharmacy or renewed by telephone (state law I believe, although the out-of-state doctor’s prescriptions had been mailed or faxed to my home-town pharmacy), meaning that I made about 120 trips of an hour or more each way, not counting stopping and waiting at the pharmacy on the way home. That’s 120 opportunities to have my wallet stolen, or lose it, or to get in a wreck in which the all-important piece of paper might be destroyed. In such a case, maybe my oh-so-compassionate doctor would have believed me and replaced the prescription that was in my stolen wallet, but the withdrawal is so severe that you feel such a risk is unacceptable. And you cannot avoid this consciousness of risk, it’s inherent in the dependency, and so there is constant anxiety, insecurity.
All medical conditions with unknown mechanism of action (such as fibromyalgia), or with no objective tests to demonstrate their reality and severity, are considered suspect both by the public and by some of the medical community. Psychiatric conditions such as schizophrenia and Post Traumatic Stress Disorder have for decades been discounted or blamed on some form of willful failure to suck it up and get on with your life. Any pain not associated with a known visible verifiable medical condition is also likely to be dismissed. Those medical practitioners who dismiss your pain also dismiss you. The more you seek help from them for this sort of pain, the less credible you are, the less seriously you are taken, until finally you may be seen as merely a stereotype: hysterical woman, somatizing patient with imaginary self-serving pain, seeker of drugs and disability.
For these reasons and others (such as fearing he’d simply cut me off, or reduce my dose and ignore any increase in pain), I never pressed my pain doctor about helping me to quit methadone until the last year or so. For his part, he demonstrated to me via a custom-mixed liquid containing dissolved methadone, of a strength unknown to me, that…what exactly did he demonstrate? After a month I came back and said my pain was worse; he said, “But the dose in the liquid was higher than you had been taking in pills.” Therefore the methadone doesn’t help your fm pain (and, implied, maybe you’re faking the whole thing). I quibble with this methodology but I was ready to accept his point and it was after that event that I made my longest most serious attempt to get off of methadone.
Over five months I cut the dose gradually (unknown to him: another result of the doctor/pusher fear-relationship is that the patient hoards medication––you’d be a fool not to––so why let him know I’d reduced the dose?) until for two months I took only a crumb twice a day, then once a day. Then I stopped altogether. The first day was okay; I’d been having various withdrawal symptoms for months anyway. But then it got worse, much much worse. For the next seven days I slept not at all. I quit even going to bed, just sat in the living room reading or surfed the web. After the first few nights my fatigue was so bad I couldn’t read, I just sat, or walked around. Nights were endless. My body was often wracked with bone pain, as if every bone were being crushed. My mind was flighty and ungovernable, my guts were gnawing as if I were starving. The methadone was right there in the bathroom but I persisted for seven days. On the eighth day I realized that 1) my symptoms were not lessening in any way, and 2) I couldn’t take another night without sleep. Within three hours of taking one of the hated white pills I was in bed asleep; the next day I felt almost normal.
The next time I saw the pain doctor I told him I’d done this and failed, and asked him how he might be able to help. Was there no sleeping medication, no tranquilizer or other drug that could be used temporarily to blunt the withdrawal? “No, there’s no magic pill,” said he. I felt like a demanding child who had asked for fairy dust to fix her boo-boo. When I pressed him, reiterating the symptoms, he said they were merely psychological.
Maybe I need a new doctor
Now I felt some solid ground under me. Research on methadone withdrawal had not yielded me much but I had found out what some of the symptoms were, and mine were common. This guy was wrong, and I had hope of finding someone who knew better. I tried my primary care physician; she told me that my symptoms were psychological. Just like him, she said that I could not possibly have had symptoms for seven days, because “even heroin is completely out of your system in 3 or 4 days.” She used the same exact phraseology as the pain doctor, whose office was in the building next door. Right, I thought. I’ve been seeing this woman for eight years and she parrots someone else’s words, not trusting my report of what I experienced. My pharmacist was more well-informed and confirmed what I’d experienced, giving me a few leads on alternatives.
The pusher drops the hammer on me
I dithered around for a few months, hesitant to step off into the unknown of a new doctor. Then came the day when my pain doc informed me blandly that he was “no longer comfortable prescribing methadone” for me since my pain was mostly fibromyalgia. His plan was to phase me off over the next two months. Sixty to zero (milligrams), zoom. I tried to be calm and asked “What about the withdrawal? I told you that it was intolerable, how are we going to get me through that?” “Those symptoms were merely psychological; it’s up to you to deal with them.” He was adamant. I was panicked. Abandoning calm, I asked him what he was going to do when I ended up in the ER. He ignored me. That was the last time I saw him. But I do hope he is comfortable.
It was the psychiatrist that I see (because fm has limited my life so much that eventually I became pretty depressed) who really came through for me. When I told this kind man about the two-month ultimatum, he took me seriously––he actually knew about the symptoms of withdrawal––and went online to research the matter further. In a physicians-only discussion group he contacted a pain doctor experienced in managing methadone withdrawal who confirmed my experience and spoke of alternatives. The phrase “managing methadone withdrawal” was like water in the desert. My psychiatrist recommended a different local pain doctor and I went to see him.
The new pain doc allayed my fears immediately. Yes, the symptoms I’d had were common. Yes, they were awful. Methadone, he said, is a synthetic opioid and it gets into the body more persistently than heroin; it can even be stored in the bone marrow, probably causing that unbearable bone pain I’d had. But there were ways to minimize the symptoms, there were choices, and he was sure we could get me through it.
Lesson #2: There are caring and knowledgeable pain doctors out there but you will have to know what you are looking for, and work to find them. Make a list of questions to ask people who recommend a doctor, and to ask doctors themselves.
From my experience, obvious questions for a prospective doctor would be:
What are the short- and long-term health consequences of the drugs you may prescribe? What different conditions may be contributing to my pain, and for each, how effective are the drugs you are prescribing? If and when I need to go off of opioids, how will you help me? How much experience do you have in this end of the process?
And ask yourself if you are willing to hand over so much control of your life, to this individual and this drug. I don’t travel much, but every time I did I worried about losing my methadone, or having it confiscated by airport security. Once when I travelled out of the US, to Chile, I was so concerned I got the pain doc to write me a letter verifying that I was authorized to have this controlled substance, this narcotic, so that I could feel less likely to end up in a foreign jail or have the medication taken away.
The first day I saw the new doctor, October 5, was the last day I took methadone. Surprisingly, he put me on morphine, a lower dose than the methadone, because it would moderate the withdrawal from the methadone and be easier to quit. (According to him, heroin and methamphetamine are also easier to quit than methadone.) And he prescribed sleep medication. He told me to call if things got too tough and he would adjust the treatment to work better.
The first two weeks were the worst; I was weak as a kitten and slept 18 hours a day without sleeping pills. After that, my strength gradually came back, and I began sleeping just at night (with the sleeping pills). I had some physical symptoms such as endless gnawing in my stomach, and constant sinus headaches and earaches, but after the first two weeks my mind and psyche began to feel completely different, as if I were coming out of a ten-year tunnel. My husband remarked on it: I was more talkative, personable, cheerful, confident. He felt he was seeing a person who had been gone for ten years. So did I.
Lesson #3: methadone does a lot more to you than just causing constipation, sweating, and sedation.
The amount of morphine was cut each month, and withdrawal symptoms lessened. On Feb. 5 the morphine ended––an anticlimax, no real difference!
I still have the sinus headaches, milder now, but if they never go away I am still so much better off that it’s hard to believe.
Life after methadone
I’m glad to see the well-known methadone side-effects go, of course; my attacks of sweating used to be so bad, even when I was sitting still, that my hair would be drenched, and outside activity would cause sweating so heavy that I would feel faint. This is much improved now, though still not normal. Then there’s constipation, which sounds like a minor thing, but when I had a colonoscopy I was told that I was at risk of getting diverticulosis because of the methadone-induced constipation.
As for sedation, at one point early on my old pain doctor put me on dextroamphetamine because I was too sleepy to do anything. It was easy to see why the amphetamines are so popular; I felt wonderfully energetic, smart, lost weight…but not a good long range life plan. Without the amphetamine the methadone caused fatigue on top of that caused by fibromyalgia.
And my old pain doctor had told me once, in an offhand manner after I asked about periods of breathlessness, that longterm methadone use could cause heart problems, but not mild ones like breathlessness. “How would I know if this was occurring?” I asked him. “You wouldn’t,” he said, “you’d just have a life-threatening episode of heart failure.”
But it was the completely unexpected and, as far as I can tell, undocumented changes that really have made life different. Chief among these are the psychological changes that I described above. I’m more outgoing, more able to engage in activities with small groups of people (though––typical of fibromyalgia––crowded places/noise/smoke/bright lights make me exhausted very quickly, so I avoid them). My depression used to edge back despite anti-depressants, but that has not happened in the three months since I went opioid-free. I feel more pleasure in life. Both my attitude and my energy are improved.
While taking methadone I must have dreamed at night, but remembered dreams perhaps once or twice a year. That made me feel cut off from a part of myself, and I am pleased that now I’m remembering dreams a few times a month.
Physically also there were unexpected results. I no longer eat between meals, feel no interest in doing so. If my stomach growls I am not seized by uncontrollable impulses to eat something. And what I eat has changed. Always a chocolate lover, I’d worked up to 1 or 2 candy bars every afternoon while taking methadone; the pull was almost irresistible, and the pleasure though short-lived seemed like something I could not give up. Now, the candy bars from last October are in a box in the pantry; in six months I’ve eaten one, and in the middle realized it was really not all that great. We got a box of See’s candy after Christmas and I enjoyed it a lot, but I can take it or leave it. The opioids are notorious for giving junkies a sweet tooth, so maybe I should have anticipated that my chocolate craving would go away. But it’s worth noting that the craving vanished during the first month off methadone, while I was still taking morphine.
Here’s one that seems very much out in left field: for years my vaginal tissues have been extremely tender and painful, even bleeding, and my gynecologist had concluded it was just post-menopausal stuff. I declined full-on hormone replacement therapy and nothing else we tried helped. Two or three months off methadone, and this began to change. No, I cannot see any causal connexion either, but that doesn’t mean that there isn’t one. It’s not psychosomatic, because I never thought about it as something that might be related to methadone. I mention this––even though I am not really comfortable discussing such matters in public––because I’ve never seen this in any list of methadone effects, and no woman would ever think to associate the two.
My reason for this post is to get more open discussion of all these issues related to chronic pain management so that others will have better information, feel less stigma about pain and opioid use, and make better decisions. I was ignorant, felt helpless and trapped, and let the matter go on for far too long; nothing can give me those years back.
Before you try opioids for chronic pain
Consider all these factors carefully before you embark on long-term use of methadone, morphine, codeine, oxycodone, and so on: Efficacy will lessen over time. Side effects, including ones you never expected and may not attribute to the drug, will increase. Dependency comes with the drug, including dependence upon the prescriber.
Educate yourself about your condition and any proposed drug. Choose your provider very carefully. Try other pain-relieving or pain-distracting methods: at any dose you can live with, opioids don’t entirely relieve pain, so you may as well look for another source of partial relief that is adequate without all the baggage of the opioids. Look for a way to feel a sense of some control over your pain: find out what aggravates it and what distracts you from it.
Don’t be too skeptical to try things like warm-water exercise or swimming, resting with your favorite music, or finding a hobby or interest that distracts you and brings you into the “flow” mental experience described by Mihaly Csikszentmihaly (whose books (see footnote 1) are a lot easier to read than his name is to spell!). “Flow” is that mental and emotional state of being so involved in a positive activity that time passes without notice. Its requirements are that the activity be something you want to do, and something that is challenging (with lots of potential for you to improve and grow) while not being so hard it’s frustrating and unpleasant; and having clear goals––my goal is to get better at this, and my next step is to try such and such. People can experience flow in all sorts of work, craft and art, and mental activity: knitting, fishing, fixing a car, playing music, doing puzzles, reading, learning something new, you name it. Think of a kid putting together a model airplane or choosing to practice something over and over. It’s basic to the human brain, but is pushed away by stress, time pressure, worry, and so on. Get back to it at times and for that time it can push away pain and stress, and give you a little feeling of control and of life being worth living in spite of pain. Things that have worked for me include reading, doing online research, bird-watching and other outdoor interests, writing, good conversation, watching movies, and drawing or painting (in which my goal is to get better, and considering where I started that is no problem! but it’s okay, I see little improvements and I enjoy the process itself, which is key).
Some kinds of pain respond to mild exercise, which can produce endorphins, distract the mind, and tone the body so it supports movement with a bit less pain. Go slow and be determined. There’s increasing research to show that chronic pain often causes depression, and depression can be treated. If you are carrying pain around every day, that doesn’t mean you also have to carry around depression. And, it’s possible to use some opioids like codeine off and on, just when the pain is worst.
Keep learning about your condition, keep asking questions, keep trying positive things that might help even a little.
None of this is meant to minimize pain, tell you to wish it away, or imply that you “should” be able to control it better than you are. Pain is real. Until people live with chronic pain they don’t realize how draining it is, mentally and physically.
But. As the saying goes, “Every day above ground is a good day,” and it is possible to make (almost) every day better.
Footnote
(1) For example, Finding Flow: The Psychology of Engagement with Everyday Life. Your library probably has some of his books, or do a websearch and read an article or two. Some lectures of his are online here.
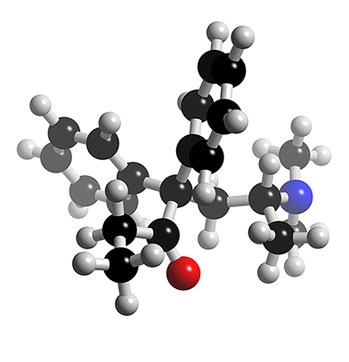
Image above: Methadone molecule, from 3dchem.com

MY DAUGHTERS BOYFRIEND TAKES METHADONE, AND HAS BEEN FOR MANY YEARS. NOW HE’S TAKING MORPHINE SHOTS AS WELL. WHEN HE RUNS OUT OF HIS METHADONE PILLS HE BECOMES AN EXTREME BUTTHEAD. IS THIS A WITHDRAWAL SYMPTOM?
absolutely it is…I am a total bitch when I miss a dose of morphine .
@Catherine Fidler,
Catherine,
Well, withdrawal can make you jumpy & nervous, sleepless, impatient, selfish, basically only interested in getting drugs to feel “normal” again. So yes, it could make him act like an extreme butthead.
But what’s the deal with him taking methadone AND getting (giving himself??) morphine shots too? Is this through a pain doctor? Pain docs usually prescribe morphine as extended release tablets for chronic pain; injections would be for those in hospital or with an implanted morphine pump. The combination of morphine and methadone is dangerous: they are both opioids and would have a combined reaction that may include stopping the person’s breathing. And of course both are addictive.
For these reasons it is very surprising to hear of someone (not in the hospital or terminally ill) being prescribed both of these powerful drugs. If he is just buying this stuff and using it then you and your daughter have bigger worries than his being a butthead sometimes. Those worries would include the boyfriend dying, becoming violent as a result of withdrawal and drug-induced mental problems, committing crimes to get street drugs, and being arrested. If he’s arrested your daughter could easily find herself in trouble with the law also. She could easily get into using drugs with him, too.
nosleepingdog
Hi, are you the one who wrote the lengthy article on methadone, and used morphine to quit? If you are, could you please email me, when I find out you are the one who wrote it, I will email you with what’s happening. Thanks so much for the informative article. Nick
Nick,
Just post your news here, so others interested can see it too.
Thanks,
nosleepingdog
Hi
in your long post, you stated, I believe that you went off methadone the first day you saw the new pain dr., oct? and in feb. you quit methadone, gradually decreasing over the 4 months or so. In you post to, I think Sandy,? you state that you were on morphine for 3 or 4 weeks, if I read it correctly. This is a big difference, can you clarify which is correct and I read it wrong, I apologize.
I am taking morphine now, taking meth., 2.5 or so mgs per day with it, this is the 4th day i have been down to this low amount of methadone. my thought is to quit the methadone completely in another 3 or so days. not feeling the greatest, but better than when i tried to quit methadone a few years ago without any help. made it for 32 days and sick every day. thanks for any help you may have. nick
sorry, in my last post, i meant you stopped the morphine, i put methadone. so where it says feb., it should state morphine. sorry! nick
Nick,
I’m sorry I hadn’t checked comments and replied to you sooner.
The time when I went off methadone, 2 years ago, was a blur, and now I wish I had kept notes about the specifics. The best recollection my husband and I have is that I was on the morphine for about 6 weeks (having stopped the methadone the day I started the morphine). I cannot remember for sure if I then went off the morphine all at once or gradually; I do remember the doctor saying that given the size of the dose, and the relatively short period, it would be easy to stop it. And of course, compared to getting off methadone, everything else is apparently easier!
This is probably too late to be of any assistance to you and again I apologize. I hope it is going well and by way of encouragement I’ll add that getting off methadone for pain was one of the best things I ever did. Even after two years I think I’m still gaining mental and physical strength compared to the ten years on methadone. This despite getting older and not doing any regular exercise routine. For me, there were no pain relief benefits to the methadone by the time I began trying to quit it; others with different types of chronic pain will have that to deal with when they quit taking methadone, so they will have face a different situation than I have.
Thank you, thank you, thank you! I had a parachute malfunction in 1988 and as a result have suffered low back pain ever since. I will keep this short as I know I don’t have room for over twenty years of pain.
I got to the point in my pain “management” that I was sick of multiple narcotics and their side effects that I said I want more relief less drug. Well, methadone was the doctors plan of choice. I am, no I was sent to come off the last of the narcotics (fentanyl patches) and start methadone next month. I am so close to tears from reading your article for many reasons. But most importantly is that I think you may have saved my life! It has been a living nightmare dealing not only with the constant pain but also the dependence and side effects of serious drugs that I just really don’t think I could go through anymore.
Thank you from the fullness of my heart! Now all I need to do is figure out what’s next for me!
Appreciatively,
Robert Wallace
Combat Medic, Airborne
United States Army (medically retired)
Re: Catherine’s comment, Burroughs, a more practical investigator into the effects of opioids than say the pleasure dome dude or some chase the dragon hipster, intimates that opium may be a parasitic plant that inhabits the host until it is reduced to a plant itself until exhausted. It is the nature of parasites to exhaust their hosts, like hag fish or tape worms. So, if boyfriend is a butthead without a confection of both synthetic and natural wit inhibitors then he is a butthead, plain and simple. Keep a close eye on your valuables – they be slipping right away. If the kid wants to be compost he can arrange the meeting himself. If he doesn’t, the pusher will.
I have been searching the internet for the last year hoping to find any answer to my problem. I have had severe back pain for years. Doctors have tried everything but surgery. I have been on methadone for two years, they just keep uping the dose everytime I complain of more pain. I have begged to be taken off of methadone because I have felt the horrible withdraw symptoms that they claim are not bad.
My family doctor will not help me go off of it, he claims all or nothing. I feel like you are the only person who knows my pain. Any advice will help?
Thanks for your input. I have a cousin that has been on this for a long time for fibro…but she is loosing her family etc. because it is taking her life over. I appreciate your information. She is in the addict mindset right now. We might have to do an intervention .
SANDY, YOU DO YOUR COUSIN NO FAVORS WHEN YOU SAY SILLY THINGS SUCH AS ” IN THE ADDICT STAGE” RIGHT NOW. THAT’S A NON-SENSICAL COMMENT AND YOUR COUSINS FAMILY ATTITUDE IS PERPLEXING, AT BEST. AT WORST THIS MAY DRIVE HE/SHE RIGHT OVER THE EDGE. JUST A HEADS UP, YOU’VE GOT TO BE EXTREMELY SENSITIVE WHEN THE ONE SUFFERING IS FAMILY.
Hi Lisa,
If you are still in pain despite methadone, then it doesn’t justify the effects of the methadone, in my opinion. Family practitioners are not pain specialists. Mine got her info from my first pain doc (the evil one!), both saying that withdrawal was all in my head.
Find a good pain specialist in your area. Possible sources of referrals are another doc you trust, or a sympathetic pharmacist—they know who is prescribing what, and hear a lot from patients. Do not sign on with a doctor who makes you feel weak or guilty or that you are an addict. You are trying to get better, willing to do something hard to get there, and you deserve support and help.
For me the pain specialist prescribed morphine for 3 or 4 weeks, just replacing the methadone with the morphine, to help with the withdrawal, and also gave me sleep medication and was ready to give me Xanax (for mental distress, extreme nervousness) if needed but I did not need it. I was weak and slept nearly all day for 2 weeks, then gradually came out of it, but never had the excruciating bone pain and mental distress that I had trying to get off without help. With the morphine and sleep meds I slept, rather than staying up for a week straight as when I tried it on my own. And I had confidence that this doctor was ready to help if things got unbearable; there IS symptomatic relief to help you through withdrawal.
Getting off the methadone is step 1 with the pain doc, then step 2 is figuring out how best to control your pain. For my particular back pain, what worked was a nerve block that silenced the pinched nerves temporarily so that I could move normally and do exercises to strengthen and unclench muscles that had been knotted up for 15 years. But no telling what will be right for your problem. Often from what I hear a combination of things helps: learning how to move better, and what to avoid; just the right exercise (in the water perhaps); relaxation techniques; muscle relaxants for a period of time; non-addictive drugs like marijuana, which is legal in my state for medical purposes. There are those who think exercise and relaxation can cure these things all by themselves, I do not agree, but they can definitely help. Some pain patients need opioids, but I think methadone is worse than the others, and the pain doctor told me that too. Methadone is cheap so it gets prescribed a lot.
When you can get help to stop the methadone, I bet you will then feel like you can tackle the back pain, feel more positive and in control. Methadone really saps your spirit.
You can do it! let me know how it goes.
Hi Sandy,
It’s good that you are concerned about your cousin, and looking for information. Be sure to keep in mind the difference between the chronic pain patient and the addict. Chronic pain patients can act like addicts, 1) because their pain is not being adequately controlled so they keep trying to get relief, 2) because they fear the loss of the medication so they hoard, try to get more, etc., and 3) because of the personality changes caused by both constant pain and the drug (methadone in this case). This does not mean that the patient is an addict, however, and treating them like one will make them resist even more, and misdirect your attention.
The pain patient wants relief. There are other methods besides opioids, although for fibromyalgia the other methods may not work too well. I myself tried 2 drugs approved for fm, which are supposed to lessen pain for some (Lyrica and Cymbalta) and neither worked. With Lyrica, I had to take such a high dose that it sedated me way too much. There is now a third drug approved just this year, Savella (milnacipran); it should be available now or very soon, although most doctors probably do not know about it.
Your cousin first needs to know that her family takes her illness seriously. This is conveyed in how people talk to her, whether they remember how she may be feeling even though, as people always tell us, “You look fine!” And whether people close to her try to give the help they can, whether it is her spouse or children taking responsibility for some of the family’s work/driving/housework, or giving her a ride if she is too tired to drive, etc.
If she feels people discount her illness, or don’t believe in it, then she is not going to be receptive to conversations about what the methadone is doing to her life. Before I ever took any pain meds for fm, I watched my life seem to vanish before my eyes: I gave up everything that was optional, only the mandatory stuff remained and I still felt like a wreck and a failure. Finally I had gone to 3 days a week at my job, and the other 4 days were not enough for me to rest up from 3 days of work. Other people had energy to go out to eat with friends on their Friday night; at the end of my 4 days off I did not have that energy.
It is not surprising that people with fm, and other severe chronic illnesses, get depressed—anyone would under such circumstances! So there is a question to look at: is your cousin being treated effectively for depression? Some anti-depressants are popularly prescribed for fm because they are associated with a reduction in reported pain, but they may not reduce the depression, since anti-depressants are different with different people. The anti-depressant I finally ended up on helps me not go into black moods where everything seems hopeless and pointless, but does not do anything for my pain. I have to cope with the pain by other means I have evolved: there are a lot of physical things I cannot do or can only do for a few minutes; I try though to keep as active as I can, use it or lose it! inactivity can just worsen things; I keep regular sleeping hours, take naps when I need them, pace myself, know that I have about 3 good hours a day (beyond the time taken for such activities as bathing, feeding the dog, washing the dishes after my husband cooks). I find things that take my mind off how I feel—reading, music, writing—and use time spent in those activities as relief. If I lived close to town I would probably try to get in some time in a pool, one with warm water if possible, because that is a relaxing and no-impact way to keep the blood flowing and the muscles working.
I don’t mean to go on and on, here. My main points are to try and understand what your cousin is going through; present positive options rather than a confrontation about methadone use; let her know she is not in a corner (“the only thing that helps me is methadone” or “getting off methadone will be awful and no one will help me”); help her find a good pain doctor who’ll help her through withdrawal and will then explore other pain-relief options. My answer to another commenter, above, gives a few suggestions about finding help to get off of methadone—it is harder to get off of than heroin. That is what my 2nd pain doctor told me, and while I know nothing about heroin, I know that withdrawing from methadone without supportive medication was flat out impossible.
You might be interested in looking at two other posts I have done, one about fibromyalgia itself
https://nosleepingdogs.wordpress.com/2008/10/11/fibromyalgia-a-personal-overview/
and the other one about the difference between addicts and pain patients
https://nosleepingdogs.wordpress.com/2009/01/25/dr-houses-writers-betray-pain-patients/
Good luck with this and good for you for being willing to help your cousin.
Your post was so informative. I have been in pain for 4 1/2 years and I still don’t have a solid diagnosis. My neurologist has thought that it may be everything from Lupus, MS, and fibromyalgia to “idiopathic brachial neuritis”. That basically means that they don’t know why I am having the pain that I do. It basically feels like someone is holding a blow torch on my back 24/7. Anyway, just yesterday I got an email from my doctor responding on one I sent to her about not being able to tolerate the most recent prescription that she gave to me. She is now suggesting Methadone. I didn’t even realize it was a medication that was used for any reason other than helping heroin (and other drug) addicts get off the drug. I have not yet responded to her email as I like to research things for myself. That’s how I came across your post. You’ve given me much to think about. Thank you for sharing your story.
Thankyou thankyou thankyou thankyou!!! I wish I could have read this before agreeing to methadone treatment. Just out of chance I decided last evening that enough was enough. After a lot of soul searching I decided I wanted to be drug free. I’m 24, been “properly medicated for pain” (yet still in loads of pain every day) since I was 14. I have taken methadone for a few years now. And I was diagnosed with FMS approx 2 yrs ago. Your information has been a great help to me. It’s wonderful to know I have done some things right! Any advice for non-drug ways of lessening the effects of withdrawl?
Much love and appreciation
Bianca
Hi Bianca,
I’m really glad you got some useful info from my post!
you asked,
“Any advice for non-drug ways of lessening the effects of withdrawal?”
Other than getting enough sleep (which for me was about 20 hours a day for the first week or so), no. I had tried on my own, as I described, and what helped me succeed finally was drugs—the month of morphine to lessen the terrible withdrawal pain and let me sleep; I think I also had sleeping pills, maybe klonopine, for the later weeks when sleep was hard. You may need anti-depressants or something like that. The pain doc I saw was up on all that and ready to give me the temporary help of appropriate drugs. Seems wrong, maybe, to use more drugs to get off of one drug, but sure worked for me!
My pain now is fibromyalgia and nothing has helped that (new drugs have been approved and I guess help some but not me) but I am happier with some pain than ever with the methadone!
Find a good doc!
Let me know how it goes.
An extraordinary service you have provided, beautifully written. What a good soul. Thank you so much. At this moment I am too tired to say more than thank you, continue with your good works and God Bless.
Sincerely,
ll
Bless you for sharing your story. There is a huge difference between true chronic pain sufferers and phony “pill poppers”. Those who pretend to suffer, or greatly inflate their pain to get meds, have so destroyed the medical system for those who require pain management. Shame, shame on you it you are one of those frauds. I sparingly use pain meds for a debilitating condition. I have access to more; however, I know there is no free ride. This blog gives an absolutely true account of drug use. Your physical body does not differ from abuse or need. You will go through withdrawl regardless. Psychological withdrawl is addiction.
I do not get high on pain medication. I only know I am on it because my pain starts going away. My personality stays the same; no euphoria. As far as I am concerned, the best pain med is Advil. The only reason why, after 15 years, I had to start taking pain meds was due to the fact I needed too much Advil, and there was a concern about it damaging my kidneys and/or liver. I thinks my willingness to try something else for so long went a long way with my doctor when I finally had to take something else. I had been under her care for that length of time so she knew I was being truthful. The one good thing about chronic pain: it feels like Christmas morning on those days I don’t have it!
Dear Lynn Bee:
Shame on you for lashing out at the sick and suffering from your soapbox of thick ignorance on the nature of addiction, the pain industry and the roller coaster suffering of others. Try informing yourself before blaming and shaming others. There’s something wonderful awaiting those who seek knowledge and experience: wisdom. Sure there are those who scam and lie and cheat. But your self righteous indignation is no less a crime. Watch that halo doesn’t slip and choke you.
Lulu,
Easy there, I think we can all relate to Lynn Bee’s feelings about the effect on pain patients, of those who are purely seeking the drugs for reasons other than physical pain. Because of our country’s hysteria about drug use, the reaction to these folks make it harder for the rest of us.
[There’s a typo in LB’s 4th sentence, “. Shame, shame on you it you are one of those frauds. ” which at first read to me as if she thought I was “one of those frauds”, but I think the “it” should be an “if”.]
But even though the people who are addicts make our lives harder, and threaten doctors who do good pain management through stirring up witch hunts, we pain patients need to extend compassion to the addicts also. Nobody sets out to become an opioid addict. Lots of factors contribute to people becoming addicts from the consumer-based society created by advertising, to social dislocation and family breakups.
Those of us who have used opioids and become physically dependent on them know better than most just what a hell it is, once your body has acquired that habit.
Wow. Fantastic post on your experience with opioids–thanks so much for taking the time to share that.
Bravo. Your article smacked the nail right on the head. I could have written it myself. I am in the care of ‘one of THOSE’ physicians. I expect a call everyday from her advising me that she is’uncomfortable’ prescribing to me.
Needless to say, I have 10 years of ‘proof of pain’, so her attitude baffles me.
My once wonderful pain doctor left the state because he felt he couldn’t help his patients like he wanted to. As a result my present doctor ‘inherited’ me. I know she wishes I would disappear.
Because of this, and other experiences with pain medication management, (travel, fear of losing medication etc.) I have been thinking about weening myself off of Avinza (morphine).
After reading your post, I think I may just give it a try.
Dear nosleepingdog,
I am so happy that I stumbled upon your website. I have been taking methadone for chronic pain for about 5 months and was VERY reluctant to begin b/c I have heard of the horrible side effects when trying to get off of methadone. However, with my doctor’s consistent urging and my nagging pain, I gave in. It has worked for my pain, but I do not like many of the side effects, so I am thinking that it is time to get off of it now. One very strange thing that has happened since around the time I started taking methadone is that I began spotting/bleeding vaginally throughout the month. I went to see my doc several times and after pap smear results and other tests, everything appears to be normal. But why this frequent bleeding and why so tender?? I have thought it must be tied to the methadone all along. After reading your post, I am convinced that the methadone is to blame. I hope to hear a reply from you so I know that you might be able to offer advice as time passes. You’ve already helped me so much. Thank you and take very good care…
Hi Kelly,
You’re the first person I’ve come across who reports that same symptom, vaginal tenderness & bleeding, associated with methadone. I would never have thought the 2 might be connected except for the dramatic improvement soon after I went off the drug (and nothing else had changed). And now, nearly two years after quitting methadone, I am still experiencing improvement; the occasional bleeding during sex quit almost at once, the severe pain got less and less, and and now I am pain-free in that department! It is not something one talks about much, I mentioned it to my gynecologist and she ruled out other worse causes but had no real recommendations. Maybe lots of women on methadone experience it and it just is not reported.
I also can say that even now I continue gradually to feel better, in terms of mental clarity and overall energy, and that *may* be slow recovery from nearly ten years of methadone. No way to prove it. Fibromyalgia-related fatigue and problems with memory, concentration, mental energy, have not gone away but every few months I notice that I feel a little better in those regards than previously. As I get older I am grateful for even small improvements!
I wish you the best in your efforts, getting off the methadone and then finding other ways to deal with pain. I hope that it may be much easier since you have only been taking it for 5 months. But definitely do have an experienced & sympathetic doctor ready to assist you. Your doctor may feel you can simply taper off gradually and then go off of it, and that may work after only 5 months of use, but be sure he or she is committed to helping you if you find it too hard to do on your own. The 3 or 4 weeks of morphine that my 2nd pain doc gave me when I went off the methadone made it possible for me, and I know from previous attempts I could not have simply “toughed it out”. Then I stopped the morphine, no problem.
Thank you for sharing your story. I do not suffer from FM but from a deteriorating situation involving a bum foot, the arthritic opposite hip, an adult-acquired scoliosis (guarding an originally ‘minor’ spinal injury) which feeds into the hip/foot problems, and assorted other spinal maladies. I’m hopeful of a coordinated approach to care that may finally bring some degree of resolution to all, later this year. Meanwhile, my PCP has advanced me over the past several years, through vicodin, dilaudid, now to methadone, as the symptoms (P-A-I-N!) and visible damage have increased and I have found I can no longer ‘manage’ – nor do I want to just manage, in a life now so restricted. Anyhow…I especially appreciated your mention of dreaming. That’s the one side-effect that I have noticed here in just the first few weeks taking methadone…a conviction that I am indeed, still dreaming (at least I’m getting an almost acceptable amount of sleep now) — but cannot remember any single aspect of any dream I might have had. Sleep had gone from being my refuge from the pain, in years past, to being made almost impossible by the pain itself. Now, with the methadone, I can sleep…but I have no knowledge of my dreams. It was at least reassuring, in that “misery loves company” way, to learn that I am not alone in my experience. I thought there was something wrong with me…besides all that known stuff, of course, LOL! Thank you again for sharing. I wish you well…literally.
Lois and others,
Good luck with your new approach. Maybe a pain specialist rather than a primary care physician, too?
It’s great that doctors are taking chronic pain more seriously; now we need to push for a wider range of approaches instead of so much reliance on opioids. There must be some for who the side effects of long-term methadone use are worth the reduction in pain, but there are many of whom that is not true. Then we have to beware of the pendulum going back the other way, as proponents of non-drug approaches can slide off into telling us, in effect, that positive thinking will do it and if it’s not working we’re not thinking positively enough!
As an aside, I live in one of the 13 states where medical marijuana is legal, and it seems to help quite a few people with intractable pain. Doesn’t work for me, but it may be worth a try.
Thanks for the reply nosleepingdog. I feel so blessed to have you as a support. I feel that the greatest accomplishment I will have survived is getting off of pain medication, once I am finally able to! I don’t expect it to be easy, but I certainly have the expectation that I won’t have to do it alone.
I was prescribed Vicodin/Norco for 3-4 years and several times I tried various ways to get off of the medication: weaning, going cold turkey, “toughing it out.” Each time the horrible, impossible effects of the withdrawl brought me back. That is why I AM CERTAIN that I cannot get off the methadone without support. And, as I mentioned before in the earlier post, the methadone has helped with my chronic pain, but I find it extremely difficult to enjoy the relief from pain because in the back of my mind is the haunting realization that without this drug ever 6 or so hours, I will be in a WORLD of pain and hurt. Freedom from chemical addiction is now more important to me than freedom from chronic pain. That being said, I have created a large support group that consists of: massage therapist, chiropractor, acupuncturist, therapist, friends with FM and chronic pain. I am lucky to have good medical insurance with my husband’s work; however, we don’t eat out or take trips of any kind…all of the extra money goes to medical bills and copays at this point. I feel like my spirit is strong and my body is stronger than ever before because of my support system and my higher power. I am just still so terrified to tell my doctor that I want to get off of the methadone b/c when getting on it she said there wouldn’t be a problem with getting me off of it when my pain was being managed. Yesterday I decided to skip a dose of methadone…within a couple hours of the missed dose, i felt miserable physically, emotionally, spiritually. Within a half an hour of the next dose, I felt normal again. Thankfully, I tried this with plenty of medication left.
The good thing is that my Doc, although seemingly misinformed or uninformed off the negative effects of opioid medication, is still an open-minded doctor who seems willing to try new things. I am preparing to go to her with my plan to get off of the methadone. Before I do, rest assured I will have several back up options for doctors who are open to treating me during the detoxification process.
Thank you again, all of you, but especially you, nosleepingdog. I’ll be in touch…
Sounds like you have put together a great team!
So, your doctor is another who is “seemingly misinformed or uninformed of the negative effects of opioid medication”—like my former pain doc and my former primary care physician. There must be one of those “gaps” at medical school, like the ones about nutrition, care of the elderly, etc.
Yes, or maybe certain doctors develop selective memory loss when the pharmaceutical companies give them “incentives” to use their products. Not too long ago I heard that the physicians were getting paid to use the drug manufacturers products…does anyone know any thing more about that? It sure would explain why doctors where I live are very quick to prescribe opiates. It’s disturbing how cheap it is to get a prescription for narcotic medication versus how much it costs to treat pain and injuries with alternative medicine, homeopathy, etc.
kelly p., regarding doctors getting paid to prescribe certain medications—-
I did a quick search on this topic (not thorough!) but found some information. It mostly relates to various “considerations” given doctors, and hospitals, for prescribing the drugs that are under patent and so very profitable for the companies. This generally does not include generic versions. As I recall my methadone was generic and very cheap; the time-release morphine I took for a while, was not generic. Things like Fentanyl patches, which I also used for a while, are extremely expensive. So the possibility that doctors are receiving anything as an incentive to prescribe certain drugs depends entirely on the particular drug.
The “incentives” include a variety of things, including the very common practice of giving samples to doctors, which does enable them to help their patients (an altruistic motive) but also makes them look good to their patients, and promotes the continuing use of the drug that is given as a sample. A relatively few doctors receive “speaking fees” for professional appearances that I suppose might be to promote use of a certain drug, or might be more general in subject but the company can still pay them. I saw a psychiatrist once who was being paid to travel and speak to general practitioners about how to evaluate their patients for depression and how to choose one of the new “very safe” drugs to treat the depression. At the time it sounded like a genuine service since depression is common and few people see psychiatrists, but as more has come out about effects of anti-depressants, and potential for inappropriate subscribing, I have seen it differently.
Payments for clinical trials are another possible type of incentive, and no doubt range from simple payment of expenses, to larger padded payments. The big threat here clearly is that the clinic/hospital/doctor have a financial incentive not to report results in a way that makes the drug look bad.
Here are some articles turned up in my brief search, including one about Vermont where under Gov. Howard Dean (an MD) a unique law was passed requiring disclosure of most of these “incentives”. Also one reference to a law under consideration in Congress to ban companies with drugs about to go out of patent, from paying off other companies not to market generics! Not sure as to status of that.
Health care reform, anyone?
News Analysis: Vermont Law Sheds Light On Big Pharma Payouts | North America > United States from AllBusiness.com
http://www.allbusiness.com/marketing-advertising/branding-brand-development/4692681-1.html
Psychiatrists Received Biggest Chunk of Pharmaceutical Company Payoffs, Vermont Study Finds
http://www.jointogether.org/news/headlines/inthenews/2008/psychiatrists-received.html
Jeff Matthews Is Not Making This Up: Legal Payoffs in Healthcare, but Who’s Complaining?
http://jeffmatthewsisnotmakingthisup.blogspot.com/2009/08/legal-payoffs-in-healthcare-but-whos.html
New Law Would Outlaw Payoffs to Keep Cheaper Generic Drugs Off the Market — Attorney At Law
http://www.attorneyatlaw.com/2009/02/new-law-would-outlaw-payoffs-to-keep-cheaper-generic-drugs-off-the-market/
Thanks for your informative article. My mother has FM and chronic back pain. She has been on methodone for awhile. She just had a car accident and had 3 surgeries. They are still trying to find the right pain meds. I appreciated all of your honesty about what you went through.
speedyrs&cs,
My heart goes out to your mom! I hope she can find an effective treatment for the back problem, then she will be in a better position to evaluate whether the methadone helps her fibromyalgia at all. It’s good that she has your support!
Hmmmm I dunno Methadone weems to work for me; I don’t really need more of it over a long time; This maybe due to individual variations; I have never tried to “kill to zero” my pain and am just happy when it happens; Of course the cause of my pain shows up in blinding bright blue on x-rays so there is no real problem of saying this caused it.
I tired and exahusted all the non-pharm “natural” fixes for my pain. ALthough the use of the word “natural” in this case because the standard opiates come from nature via a plant!
I was originally on Duragesic which worked very well. I have in the past had acute repeating pain from kidney stones and got dependent on oxycodone but broke vfrom that with moderate effort; It was after the pain from degenerating joints on my left side became chronic and trying every new age “natural” trick that I decide oh well pharmacuetical pain relief might be better. Celebrex and Bextra did nothingand were expensive. After I got to the point where I couldn’t work that everything went downhill and I started drinking heavily which I had never done before. I had reasoned that one does not have to have atrgue with someone at the package store if one wants a 6 pack of beer.
I tried and tried all the distraction stuff an new age modalities and found they just didn’t work for me Anyway after a big disaster I was put on Duragesic by a surgeon at the hospital and it worked so well that the Psych where I was shipped off too for about a week thought that I was depressed because of pain and pained because of depression.
I was switched to Methadone and found it worked about 70% to 85% as well as Duragesic. I needed no “breakthrough fast acting opiates such as oxycodone” . With methadone I do; I find Methadone easy to adjust up and down and curously if one likes the pleasant effects less is oddly more, because for me above 60mg a day the pleasnt effects go away.
This is all very curious to me how people can come at things from very different places. It maybe that we live in a “one size fits almost all” society.
I agree people should read uop and consider what they are doing if they go onto chronic opiod use of any kind. Being physically dependent is a big change. One has to consider is it worth it. In one’s heqart of hearts I think opne will find the answer.
By the way testing the waters I found that Methadone withdrawl is milder than other opiate withdrawl but the idea that it goes on for 3 to 6month is not cheering. N.B. It took me 4weeks to break free of Hydrocodone and Oxycodone dependence and that was doable but I did not have chronic pain at that point.I might try to break from Methadone if the pain would go away but it’s the pain that keep me using methadone at a mean done of 50-60mg a day, good periods 20-30mg/day and bad periods 80-90mg a day; After about 70mg?? every day for me the pleasant effects go away and then I lose the signal I have always depende on. Which is take enough so you feel it but don’t get blasted. But oddly for me the closest thing to a stable dose, going in early, no cutting down on my activities came from Duragesic 50mcg/hr change every days pain patch and I was stable on that for 4 years.
The sad thing is if I were rich I would probably get put on Duragesic again as it it was the best and did it’s job and didn’t get ion the way. N.B. I got neither constipation nor reduction in sex drive on Duragesic and I woke most morning glad to be alive which was something I had lost when all the pain came around….
Have Fun,
Sends Steve
Maybe it’s just me. I have never experienced these pleasant effects that people are after. I was of the assumption that if you have pain, it helps the pain. If you take more than your pain warrants, then you get pleasant effects. Again, this was my assumption. I never understood why people were drawn to these meds for such a street price. But my doctor said that I am not feeling the classic euphoria because my meds are taking care of pain.
Hello, thanks for your wonderful story – it made me feel like perhaps I will have hope for some semblance of a life (which I don’t have now). I have been on 240 mg. of Methadone a day (I take eight 10 mg. pills, 3x a day) — a dosage which I’m told is very high and always seems to be higher than everyone else’s. I have a very high tolerance to pain meds — it takes alot to have any effect of my pain. Even at this outrageous amount, I am nearly always in constant pain. I suffer from several chronic diseases — too many to list — but I think that I could have a near-normal lifespan if not for all these drugs. I also take Lorazepam for muscle spams and quite a bit of Fioricet for daily migraines. My pain management doctor has me ‘over a barrel’ and knows it, doesn’t take me very seriously and frequently mentions dropping me as a patient if I don’t ‘comply’. I can’t even apply for state medical aid or I’ll be dropped (and I can’t work anymore and am dead-broke). I have worn out my welcome by borrowing from loved ones and my self-esteem has vanished. I think about suicide every day, several times a day. I want my life back!!!! I don’t know if it’s possible, where I can start, or how to get enough energy to even my myself presentable enough to leave the house. My energy level is at about a 1 and I am extremely depressed. Every other so-called ‘pain management doctor’ in my area just gives injectables and doesn’t prescribe pain meds (not that I want more of THEM). Many times I’ve considered going to the state psyche hospital but am in terrible fear that they would only induce a cold turkey withdrawal, and death seems a MUCH better choice if given one. Do you think that I have a chance for a ‘normal’ life again? I used to have a VERY good one until I made a very stupid choice. Thanks again for your post – I know it has helped many.
dingbatqueen,
There is always hope. Human beings are very strong, and can make changes!
That is a high dose of methadone, and it is bound to be affecting your energy level, mood, and lots else in your mind and body. Also, if you are still feeling a lot of pain you’re getting all the negatives from the drug without, perhaps, enough relief to make it worth while. You didn’t say what the pain condition was (if there’s more, in addition to muscle spasms and migraines, not that those aren’t plenty!); getting a clear idea of the cause(s) of the pain is necessary. Only then can you explore other pain treatment options.
The other necessary thing is even harder, finding a competent pain doctor that you can work with. One who threatens you does not fit that description, obviously, yet I know it is difficult to find good pain doctors, and very scary to change. I worried for years about looking like a “doctor-shopper” or drug seeker. My pharmacist was a good resource because he knew who was prescribing what and talked to a lot of patients in the course of his work. Another doctor also helped me find the right pain doc. If you can get a line on a better doctor, it would be worth going some distance for a complete evaluation of all your pain sources and medications.
As another commenter, SteveK, notes, methadone can work well for some people, even be their best choice, I cannot deny that. But every person’s situation is different: what causes their pain, how bad it is, and how it responds.In addition to individual differences, there are others: I have seen research indicating that men and women differ in their pain receptor systems so that drugs that work mostly on one type of receptor relieve men’s pain much better than women’s pain. A drug now approved for fibromyalgia pain, Lyrica (a form of pregabalin) evidently works for some people but for me I was way too sedated before any relief began.
So my view is that pain treatment is highly individualized. I’m glad that methadone works for some people, but that doesn’t mean it’s best for you or me specifically.
SteveK had no success with “all the distraction stuff and new age modalities” ; still, they may work for some people especially in addition to another conventional treatment. If I’m in severe pain then I doubt that relaxation and imagery are going to help, but if the pain is reduced by some other means, all that “distraction stuff” may help me deal with the remaining pain, or alter my attitude so I can gradually expand my activities, and that can help a lot.
But back to your situation—right now you are feeling pretty trapped, with a threatening doctor and the risk of losing even that if you apply for state medical aid. Yet I believe that in most states there are now laws requiring pain doctors to either continue treating you, or make other arrangements. Information is power. Without it you are likely to be on a downhill path. Try to find out about what options there may be: support groups for chronic pain or various conditions may be a source of information about a better doctor, pain treatment options, about what the state medical plan can and cannot do for you, about getting social security disability (which comes with Medicare). Organizations such as those that help disabled people, as well as people with mental health problems like being suicidal due to pain, may be another thing to try, as they deal with all these issues. And at this point you are disabled—we hope it is not permanent, but until something changes, you really are disabled. Make a list of possible people/places to ask for help and information, then sit down with the phone book and start. Hospitals can often tell you about support groups and agencies.
Keep focussed on your goals, don’t get sidetracked on just telling people your story—you want forward progress toward change, not just sympathy.
Of course, the web can be a good source too. I found a scoliosis support group for a relative, googling “scoliosis support, Town, State”. Then it was up to her to make the call, find time to go, listen to the people there and decide who might have useful experience, useful suggestions. And then keep going, toward her goal of pain treatment without spine surgery.
It may seem like a huge task and it comes when you are at a low ebb of energy and everything else. But you need to do this for yourself and it won’t get easier by waiting. You need to know more about your choices, find the right people to assist you, and stay with it. Make a list, decide what you are going to first, then next, etc. Do something on it every day. If you do, you’ll begin feeling you are making some progress and that will help you keep going.
If you can make some other small commitments to yourself, like “Everyday I will get out and walk around the block (or just down the sidewalk a little way)”, something that represents a positive change no matter how small, and keep it up, that too will strengthen you. I went to a fibromyalgia event once where a nurse was telling people to walk and do stretching exercises, and some people said they couldn’t even walk half a block. She replied, “Can you walk around your kitchen table? Good, then start with that!”
You know you are in a bad situation, and staying there is really not an option—things will get worse. So resolve to be your own best friend and do some things every day that help your plan, that make you a bit stronger, that give you a bit of joy. Keep in mind your goal, and maybe keep a record of what you do to get closer to it, again a way to remind yourself and reward yourself about progress made. Even an unproductive phone call is action, is better than not making a call. So, you did that call, now you can do another, try another possibility.
Let us know how you’re doing!
Just a P.S. on my post — at my present dosage I don’t feel any ‘high’ and still have trouble sleeping at night (mostly due to pain). One would think that I sleep all of the time but I don’t. As I mentioned, it seems to take higher doeses to have an effect on my body. Just an FYI in case anyone thinks that I must sleep all of the time.
Dear dingbatqueen,
This is not the author responding to your post, which you have probably gathered by the name, but I am another person who also has made posts. Because of doing so, I receive emails anyone makes a post, which is how I was able to read yours. I wish I could help answer your question in regards to whether or not you would be taken off your meds cold turkey if you went into a psychiatric hospital…hopefully nosleepingdog will have some more information in regards to that…she has been a blessing to many of us, including myself even if she doesn’t have all the answers.
I must say that I feel for you, so very much. It sounds like you are in a very painful place. I am also on methadone and have been for about 8 months. I take 50-60 mg of methadone daily along with an antidepressant, celexa (20 mg a day). I don’t have anywhere near the pain issues you do and so methadone has worked for my pain. But I have suffered from major depression and alcoholism and addiction for several years, prior to getting clean almost a year ago. December 24th, 2009 I will have one year!
What I did in early December of last year was hit my rock bottom. I won’t go into too many details, but I knew I needed help and I, too, was too terrified to go into a hospital. I am lucky to be covered under my husband’s health insurance, (although I believe many places will take you w/out insurance), so what I did is I looked in the phone book under counseling services, specifically addiction specialists. I found a place in town that I thought offered counseling services for addition (like one-on-one therapy) and I made an appointment to see someone right away. I was terrified and almost didn’t go, but thank God that I did. After an 1.5 hour intake, I was given the recommendation for outpatient treatment. –Keep in mind that I told them that I would have to continue my pain meds (norco was what i was taking at the time) because of my chronic neck pain and headaches, and they allowed me to do that because I was there voluntarily and not through the court system. I remember feeling very surprised that an outpatient treatment program would treat me even though I was taking narcotic medication daily…and admittedly abusing it. They told me that their goal would be to have me work on taking it as prescribed…that never happened, until I went on methadone — I have to mention that during this interview I was 100% honest about the questions they asked me. I have never been honest in situations like that before. I knew that if I was serious about getting the help I needed, that I would have to be as honest as I possibly could. And luckily God gave me a very cool counselor who i felt i connected with right away. :O) So, to recap, at the end of the interview it was recommended that I attend outpatient services. Actually, the counselor’s exact words were: “I believe that you would benefit the most from inpatient services, but I know your life makes it so that you are unable to commit to that at this time. I was never able to receive the GIFT of inpatient either, but outpatient I was, and I have been clean almost 9 years because of it.” I can remember leaving there that day with hope in my heart for the first time in a very long time. And so, this was the door which opened me to a new life full of hope, love, support and freedom from chronic pain and addiction! So much of our physical pain is made worst by our mental and spiritual state.
I share my story with you so that I may offer my experience, strength and hope. I don’t think you mentioned that you have issues with addiction, but the meds that we are put on are so strong and addictive that even if you aren’t an addict, you often and in many ways live the life of one. I wish the best for you and I believe that if you are willing to do what it takes and believe in a power greater than yourself, you will be able to live a new life…you have reached out and admitted that you are helpless. That is the first step in getting better. I will keep you in my prayers and I hope to hear from you again via post in the future…
Be blessed ~
-Kelly P.
Kelly,
Thanks for this account of your experience! It helps others so much to hear from someone who has been through it, to know that “very difficult” does not equal “impossible”. And congratulations on your upcoming one-year anniversary, of being in control with your meds!
Dear nosleepingdog, I am a chronc pain paitient taking high doses of pain meds.
Not morphine but was had a provider try to put me in it. Have several issues as i was hit by a car years ago. I have been on pain meds since 1997. I have tmj (jaw joint problems. I had a joint replacement and then had it taken out . Right now I have
no joint on the right side of skull. My left side is scarred up. I need double jaw joint replacements. I also have knee problems and need a knee replacement, maybe 2.
I have nerve entrapment on the side of one leg. I also have had spinal sugery and have scarring(?) nerve damage)? and pain in legs and feet. I had a calcified stylomanbiular ligament removed. It goes from jaw to back of skull to jaw from going to far forward. That is enough. You get the picture. Maybe one of these conditions someone reading will relate. The Lord changed my life about 30 years ago in my livingroom while praying. So I would say prayer first above all. Then one day at a time.There is a very interesting article in the tmj letter talking about not addicted to pain meds but addicted to pain relief.
Don’t get the wrong Impression, I am not telling to run out and get pain meds. I want so much to be off but some of my pain is very intense. I am taking one day at a time with goals and the rest is in HIS
hands. It is very important in my opinion
to manage your health care as nobody is going to do it for you. I am in this place somewhat by dealing with the wrong docs etc. Thanks and blessings to all, TJ
I also wanted to add for the one that you mentioned about going on disability. It takes 2 years after you go on disability
to get medicare unless you are old enough for medicare anyway which means you would already have it. Thanks, TJ
Hi NoSleepingDog,
I had hoped to get off the methadone a few months ago, but I did not end up having the support that I will need to help with my daughter while I am detoxing off of the methadone. I will, however, have it starting April and therefore, I am looking at getting off of the methadone then. I have weaned myself down from 60 mg to 40 mg daily, but find that if I take less than 40 mg, I begin to feel the affects of the withdrawl. I am just so eager to get this out of my body, but am also very fearful of the process of withdrawl. I just want to make sure that I have as much information as possible. Thankfully, I will have your suggestions and story to keep in mind. I just wanted to clarify something…I think you said that you were prescribed morphine for 4 months to help with the withdraw from the methadone, but I also believe you told me that you took the morphine for just over three weeks. Did you gradually take less? And how long did you continue to need the sleeping medication for? Again, I hope to gather as much details as possible before I talk to my doctor and/or look for a doctor who specializes in helping patients get off of methadone. I am unsure of whether or not my doc will prescribe me morphine, but have been informed about a doctor in the area that helps patients get off of methadone. Your experience, strength and hope have helped many of us. I look forward to writing my own blog once I make it through this journey.
Be Blessed!
-Kelly P.
kelly p.,
You’re determined and planning ahead, a good foundation for success!
My memory of how long I took the morphine is that it was about a month, beginning the first day I saw the new pain doc. I stopped the methadone right then and substituted the morphine, a low dose, to help with withdrawal. It prevented the terrible bone ache I had experienced before when trying to do this on my own, and maybe helped me sleep, which is mostly what I did for about two weeks. I was not on the substitute morphine long enough for stopping it to be a problem.
After the first two weeks I began having trouble sleeping and the doctor prescribed first one sleeping medication, then when that did not work, another. I finally ended up on trazodone which I had used for sleep before I began taking opiates for pain. And I still have to take trazodone to sleep—only 25 mg.
I would like to get rid of it too, but since (with the fibromyalgia) pressure = pain, lying in bed is painful and keeps me from being able to sleep, so perhaps I am stuck with some sort of sleep medication. It’s a generic (cheap) and has been used by a lot of people, without problems as far as I can discover. When I was taking it the first time, I took a higher dose for several years. When it overlapped with the methadone the combination made me very foggy and confused, had trouble driving, so at a doctor’s recommendation I stopped the trazodone. I had to taper off it gradually because I felt a withdrawal from it too, which I was told was unheard of. Perhaps it was the combination with the methadone. Took a couple months.
One of these days I’ll go back to the pain doctor, have a look at my records, and make note of things like exactly how long the morphine replacement lasted. At the time, I was not in very good shape for remembering well or taking notes!
I haven’t seen that doctor about post-methadone pain management because there isn’t much to be done about fibromyalgia pain, and it is not as acute as the back-spasm pain that drove me to methadone in the first place.
But that is of course something you’ll want to talk to your doctor about: pain management after the methadone.
I can say that some self-help/coping activities that are applicable to chronic pain conditions have become either possible, or easier, after the methadone. For example, I started a walking program this past fall for exercise and in four months have worked up to over 2 miles of brisk walking, every other day. That is far more than I have been able to do for over ten years. While taking methadone I tried walking but the subsequent increase in pain and fatigue was huge and I could never keep it up long enough to see any gains. Also the methadone made me sweat like a horse with even mild exertion, and get so overheated I would feel dizzy.
Walking (or other tolerable exercise) won’t cure chronic pain or fm, but it does stop the gradual decline of muscles and the cardiovascular system which if allowed to persist will cause increased disability and hence make one’s life worse. It gets me out, improves my mood, and while at first it seemed to suck up a lot of my available energy for the day, that’s getting better and I often feel somewhat energized when I am finished.
I was skeptical; a lot of the “get out and exercise” advice is given insensitively, without realizing how extremely difficult it can be and how small the tolerable amounts may be. And then some sources seem to think that increased activity shows you’re “all better now”! Nonsense! But once I was able to keep at the exercise, starting low and working up, it has been very positive. We can’t cure ourselves of these chronic problems but there are usually some things we can do so that they don’t limit us so much, and so we can distract ourselves, have a feeling of accomplishment, and so on.
I’m glad that my experience can be of some help, and very happy to hear that you’ve gotten some support to take care of things while you get off of methadone. The first 2 weeks, I doubt I could have fixed myself a meal much less care for anyone else.
Please let me know how it goes! My thoughts will be with you in April and beyond.
Thank you so much for taking the time for this blogg. You have helped me decide NOT to go on methadone for my Pain Management. My Dr did prescribe it and I tried it for a week but could not deal with how it made me feel and the heart palipitations caused anxiety which I then needed my xanax which then sedated me even more creating a vicious circle that I didn’t want to be in.
My degenerative joint disease and fibro has been managed for years with loratabs 7.5 which has now been increased to 10 mg 3-4 x a day. I go as long as I can in a day before taking any thing but still live with some pain and a fear of being an addict. Your post has been a lot of help in my evaluating whether to go on to such a addictive drug. Hopefully a new Pain management drug will be on the horizon for every one with out all these horrible side effects. Some times the cure is worse than the disease and I think methadone is one of them.
Yes! Walking is one of the best things I can do for my pain. Luckily I live in a moderate climate, which rarely gets over 75 degrees because I also sweat profusely from the methadone. Actually, that is one of the top few driving forces behind wanting to get off of methadone. I can’t believe how intolerant to heat I am now, and how much I sweat. In terms of sleep medication, I have tried Trazadone in the past and both times it gave me a horrible headache. So that one is out for me, but I am prescribed ativan for anxiety and for sleep and only take it every once in a while currently. My prescribing doctor for the Ativan writes the prescription for 1 mg per day, so I am fairly certain that I will have the access to ativan for sleep. I know that it is also an addictive drug that can be difficult to get off of, but I have gone on and off of it several times without much discomfort, probably because I have never taken more than 1 mg daily.
My continual thanks to you and the others who share their story…it helps me to feel less alone in this.
Be blessed!
-Kelly P.
I injured my back at work in 2002, my story is much the same as those I have been reading here. Vicodin/Soma/therapy. I have not had a pain free day in almost 8 years. After 2 years on the Vicodin, my Dr. bumped me up to Percocet, still no help. She eventually put me on Fentanyl patches, starting at 25mcg. Over the course of 6 years, I was up to 100mcg. I have moved in the last 2 years, and found a different Dr. Back in June he gave me a choice, patches or pills, not both. I chose pills, no insurance and the patches are about 300.00 a month. I knew the withdrawal effects of Fentanyl, because they start to kick in very quickly when the patch is used up. My Dr. was ready to take me off the patch that day!! I told him no way, and we worked out a gradual lowering of mcg over a period of 4 months. During that same visit he also reduced my meds back down to Vicodin/Soma x2 a day. One every 12 hours. It’s true about watching the clock and being a slave to the meds. I went back yesterday for my monthly refill and asked him to increase the meds to at least 3 a day, as I am in pain all the time and my present dose leaves me in greater pain at least 6 to 8 hours a day. He was unwilling to increase my dose and suggested methadone as a pain reliever. The thought scares me to death after going through the Fentanyl withdrawal, and after what I’ve read here, I have no idea what to do. I asked him what his goal was for putting me on methadone, and he said to get me off of narcotic drugs! I am really confused here. Any thoughts or suggestions would be greatly appreciated.
For anyone being treated with narcotics for pain and wanting to come off them as painlessly and prudently as possible, I wish to share with you what has worked best for me. KADIAN is a new form of morphine that is taken once a day! It comes in various strengths, the smallest dose is 10mg HOWEVER, the good news is that this medication can be compounded, meaning the pharmacist can break down the dosage by 1mg increments, if necessary. This medication has no rise or fall, that I have experienced so there’s no feeling of discomfort prior to the next scheduled dose. If you are patient and willing to come off slowly, think about this medication to replace the current narcotic you are using, even if it’s another form of morphine. I believe that Vicodin, Oxycontin here in Canada, is the MOST addictive form of narcotic pain medication on the market and that in time it will be forced off the market. There are a slew of class action lawsuits pending against the makers of this drug, and rightly so. I also believe that one day the lid will blow off the “pain industry” (pharmaceutical companies) promoting and prescribing narcotics, especially these highly addictive forms of narcotics for “chronic pain”. They have tried to tell us we will not become addicted if we’re taking the drugs A) for pain and B) as prescribed. I will share that when I was taking Oxycontin, my dose peaked at 400 mg daily before I sought help. Apparently this is equivalent to 800 mg of morphine. When I was switched to morphine my dosage was dropped by 50 %, or half, to 400 mg morphine every 24 hours, with no waithdrawal. The tapering has been gradual with a few setbacks. Today I am taking 30mg KADIAN daily, once a day, every 24 hours. I am now also on Clonidine twice daily and a variety of supplements, when I can afford them: Vit C, D, Calcium/Magnesuim, Super Omega 3. Melatonin at night, Calms Forte (an excellent homeopathic anti stress remedy). Extra strength Tylenol (plain) for pain; NSAID for pain. I also take elavil 30mg for pain and to help restore REM sleep. I have started an antidepressant. I have been withdrawing for two years. If anyone told me I would be suffering on these meds for over three years I would never have believed it. But here it is. One day at a time I am getting off them because I want to. I have been diagnosed with lupus, arthritis, sjogren’s, osteoporosis, gastrointestinal disease and suffered chronic pain for years. Have also had many broken bones, recently five fractured ribs plus two vertabrae fractures, degenerative disc disease, with ruptured cervical discs and am a bilateral breast cancer survivor. I cannot remember half the things I’ve been “diagnosed” with. These narcotics have given me long reprieves from pain however the anguish of withdrawal and depression that goes with them seem more debilitating at times than the chronic pain I’m treating. During episodes of acute severe pain, be it from injuries or surgeries, or acute bowel disease, I could not have survived without them, or so I believe. Then again, look at Haiti and all the untreated pain and suffering these poor people have endured! We do what we have to do. I look forward to being free again, one day soon. Best wishes to the all of you on your journeys back.
i just wanted to thank the person who opened up and shared all there terrible experiences with us. i also have been on every pain medication under the moon, and also have many medical problems from severe fm which was diagnosed when i was in my early 20’s . i have migraines frequently and i have seizures. and many more health problems, including in feb. i stared coughing up lots of blood and had to be in icu for several days with lots of test and no answers. i have to take 50 mgs of methadone a day, and 40 mgs of klonopin ( for seizures), 40 mgs of oxycontin er, vistril 50 mgs for nerves and stomach problems and 50-100 mgs of demoral for breakthrough pain. i know this is alot of meds and i only take the methadone in am; then klonopin , vistril and oxycontin on a daily bases some days i have to take my full dosage of K<V<and OC and some dys only part of the dosage recomended, i hope i am making sense with all this my question to the person who started this blog is do you rember the name of the morphine medication you were on to help you get off of the methadone because i'm so tired of taking it and i have been on and off of it for 15 yrs. i even had to be placed in a rehab about 5 years ago in Florida which at the time i lived in ms. and while i was there for 30 days trying to get detoxed off the methadone guess what they gave me to get detoxed METHADONE didn't work and i had to be rushed to hospital 2 times b/c i started having convulsions and i had a $40,000.00 bill just from rehab. i have been in 4 different rehabs trying to get off methadone and even tried to taper myself which was very dangerous. i truely hope you can remember what they gave you so i can tell my dr and by the grace of God, i to will have this methadone out of my life. i will tell you that methadone can stay in ones body, bone marrow for up to 2 years and that is what a methadone specialist told my family, that is why they normally give you neurontin for the bone pain and clonidine or catapress to help with the racing heart and they also give vistiril to help with your nerves and to help you sleep or atleast that is what i have been given at every rehab i have been in to get off of methadone. i'm sorry this has been so long but i have trouble trying to relay my thoughts and even asking a question can be difficult. thanks , gina
Hi Gina:
I’m not sure who you were addressing your question to about what form of morphine was used for withdrawal, so I want to tell you what I’ve been using and you take it once a day: KADIAN. It’s been very helpful. I sure hope you have medical insurance because I can’t imagine what your finances have endured given your medical history. Perhaps you could find a true addiction specialist MD to guide you medically through the withdrawal. They say addiction is a three-fold disease: physical, mental, spiritual. This has proven true for me and I believe in the power of daily prayer to work the miracles needed in recovery from addiction. Find yourself the spiritual mentor(s) as you line up your other ducks in the medical and holistic communities to help you through this. We must learn to live one day at a time. All things are possible to those who believe. Ask for help. Blessings to you. lulu
lulu, thanks for the info. i have been to a true addictionoligist and he was the one that specialized in methadone treatment and detox he was the one in jacksonville, florida. no luck there. i was hoping the person who started this blog i think NO SLEEPING DOGcould remember what form of morphine medication they were placed on during their detox or weining off of the methadone . or anyone out there just like lula who was nice enough to tell me what helped her because i’ve tried so many other medications to no avail on getting the methadone monkey or should i say curse (for me anyway) off of my back and out of my life for good.. god bless!! gina
Gina,
Sorry it has taken me a while to reply. KADIAN was the form of morphine that I was given, for 4 -6 weeks, when I went off morphine. At the end of that time I was able to stop the Kadian just like that, without having to do a gradual reduction of dose, because I only took it for a few weeks. It helped suppress the worst of the withdrawal symptoms, such as the sleeplessness and the bone ache. I remember it was expensive but the doctor gave me some sort of free coupon for about half of it.
Your case is going to be more complex than mine, with the different drugs that you are taking. Is there a single doctor overseeing everything you take? Sometimes when multiple doctors are involved, prescribing different drugs for separate medical problems, the drugs become more harmful than helpful and the doctors lose sight of the bigger picture, which is the patient’s overall welfare and condition. Somebody needs to be in charge who knows & cares about drug dosages & interactions, and can consider alternative approaches. And the patient needs to judge whether medications—even when working as they are supposed to—might be worse than the symptom they’re treating.
You mention having had several drugs to help with methadone withdrawal. My best recollection is that all I had was the Kadian and something to help me sleep, klonopin or xanax. And sleep I did, for a couple of weeks. I will get the details of what I took and for how long from my former doctor so I can post them. At the time I wasn’t remembering too well!
Your drive to get off the methadone is clearly very strong and I hope this time you have the right help and medications to succeed!
Hi! Thx for writing the article. I have been taking M for 5 years and have alot of the same worries that u do. I’m terrified to travel out of the country and my girls r always begging me to go. I have a huge difference….I am NEVER hungry…..go for 3-4 days w/o eating anything. Aboslutely NO appetite. I’m forcing myself to eat something once a day. And I’m horrific at drinking….go 2-3 days with NOTHING to drink….which of course only exacerbates the constipation immensely!! Thx again!
Max,
I hope you’ll think about ways you could get off the methadone, solve the pain problem another way, because it sounds like the drug is out to kill you. Not eating or drinking, hard on the kidneys, the bones, all the organs really. If you found my post, you’re concerned about the methadone…do you have a doctor who’s knowledgeable and trustworthy, who could help you with this?
hi, everyone, hope this finds y’all doing good. i wanted to thank the people who took the time to answer my questions. i also wanted to let you know that i only have one primary dr. and he was to scared to place me on the kadian to help me get off the oxycontin and the methadone. please just keep me in your thoughts for this is a hard time for my family we just lost Granny she was in her 90’s and she was my biggest supporter and never was ashamed of me like so many are. it’s been a blessing to find this website. good luck and may your higher spirt help you! gina
My husband suffers from chronic pain, fib and migraines, for over 20 years. After many years of every med in the book pain clinics and surgery, he was given methadone two years ago. He is slowing slipping away and he is now afraid, he is paranoid is this also a symtom, the migraines are worse, we are in Canada where do go now
Mary,
I totally relate to your husband’s pain and fears. My migraines have gotten worse over the years and now are totally uncontrolled. My pain management dr says with mine being due to heredity and other factors that a nerve block isn’t possible. My pcp wanted to do botox which has been shown to give 3-6months of relief…which I was willing to try anything but of course they’re so costly and my insurance refused to pay and only sees them as cosmetic it was a no go. I just can’t live with them without medication and don’t know what I would do if I had to try. I commend you for standing by him and being understanding….not alot of people get that and to feel like you’re alone makes us feel so much worse. I pray that you and your family find a life with peace and without pain! Take Care
I’ve suffered with uncontrolled and chronic migraines for over 20 years. I also suffer from depression and now arthritis and high blood pressure. After seeing numerous Neuro doctors, I was finally sent to a Pain Management Dr. after having to practically live at the ER. Of course, where you get the junkie treatment which makes you feel worse than you already do. I wanted to be honest with my Neuro Dr., but not sure how he would respond. The pain and symptoms are UNBEARABLE! I vomit, am sensitive to light, sounds and smells with my migraines. Have gone thru cycles as long as 5wks.(meaning not 1 day without a migraine and all the lovely symptoms). No one understands how bad I feel…except my husband and my parents. I’m a mother of 2 and they’re over 18, but they just think its simple and I should just go on with my day to day activities….but I’m not able! Being a very active wife and mother before has caused the depression to become so bad at times, I feel like I just don’t know how I can go another day like this and beg for God’s help controlling the pain and for an answer for help. My Neuro dr tried putting me on morphine, but it causes me to vomit so he took me off if and sent me to the pain management clinic. My doctor is nice and seems to understand how I long for relief and for a life of not having 2-3 migraines a week that last for days. He did however prescribe me methadone and I use dilaudid for break through pain which was GREAT! Now after almost a year…the migraines aren’t being controlled like they were and I’m afraid to talk to him for the fear of being seen as addict! Not to mention all the things I’m hearing about methadone has me concerned ALOT! My blood pressure is staying elevated which is triggering the migraines as well and my pcp has me on 2 bp meds a day, but still with a migraine it causes my bp to stay up and with bp up it triggers one….feeling like where do I go now. I’m so glad to see this article, but am so fearful of what’s going to become of me and my pain. If you can offer any suggestions, I would greatly appreciate it!
Chronic Pain Sufferer in VA,
[reply sent via email]
Hi NoSleepingDog,
I am a chronic pain sufferer with advanced hip and knee arthritis as well as nerve pain in my legs which were fractured 24 years ago. I have been on hydrocodone and oxycodone for over a year now, and have just began seeing a pain doc. Guess what he prescribed me? Yep, Methadone. 5 mgs a day, twice a day. It doesn’t seem to be controlling my pain nearly as well as the opiates, but my tolerance for the opiates was increasing. After reading your story I am extremely worried to continue taking the methadone. Any thoughts??
KC,
Here’s a good resource on nerve pain: http://www.theacpa.org/uploads/documents/chronicle_summer06.pdf
nosleepingdogs
KC,
Your tolerance for methadone will increase too.
The nerve pain and the arthritis pain may be amenable to different treatments. Can you do some research and have some ideas to talk over with your doc?
Here are a couple of things that occur to me:
1. use of methadone temporarily, then return to the opioids and see if the break in use has reduced the amount needed to give you relief. (I am not a doctor! but from what I know this seems feasible to me.)
2. explore with your doctor non-pharmaceutical forms of treatment. I’m not up on this, but two I do know about are TENS units (electrical stimulation units you wear, and the electrical current confuses or interferes with the nerve transmission; here’s a short explanation, http://arthritis.about.com/od/assistivedevicesgadgets/g/tensunit.htm) and also nerve blocks (injection into a nerve that blocks it for a period of months; there may be longer lasting ones too).
3. Is the leg nerve pain possibly treatable with surgery? Is it pressure on a nerve, or can they tell?
4. This sounds off the wall, but for arthritis there are a lot of people who have decreased pain from what doctors would call folk remedies. I have worsening arthritis in my hands and do get relief from the grape juice and pectin remedy. I put a packet of liquid Certo in a jug of purple grape juice (not drink, but 100% grape juice) and drink about 12 oz a day. If I miss a couple of days I feel the difference. It does not help the swelling of my joints but has reduced the pain by about 80%. Check the Peoples’ Pharmacy online, they also have a newspaper column. They are more judicious and informed than, say, the mailings from Prevention magazine. Another that works for some is golden raisins in gin, and no you don’t drink the gin, just soak a month’s worth of raisins in a little jar and eat about 10 raisins a day. Didn’t work for me.
5. As far as what your doctor can do for you, my thought is to explore potential treatments for the 2 conditions separately. Methadone/opiates are the easy one-size-fits-all response to pain, and for some that is what it comes down to, they can’t function without relief and nothing else works. But I’d explore other choices. And remember, whatever you can do to lessen one of the sources of pain, may make the other pain easier to treat or easier to put up with. Attack it from multiple points. Even small gains can make an appreciable difference.
6. I used to be a skeptic about exercise for fibromyalgia, and I still think there are a lot of people for whom any consistent exercise is not possible, and that this again becomes a way for doctors to deal with difficult conditions, by putting it back on the patient. But. There’s evidence that exercise reduces pain in arthritis, and it can prevent progressive loss of function and strength, and it has many benefits for body and mind.
When I am concentrating on something that I really enjoy doing, my pain recedes. If I am inactive and depressed, the pain feels worse. To me that says that there’s a possibility to attain the lower level by means that have nothing to do with treating the condition. Exercise stimulates blood flow, makes your brain work better. Being active gives you more to think about, distraction if you will, and provides satisfaction of accomplishment.
Your injuries and arthritis may make it impossible for you even to walk, but if not, that has been the best for me. Cheap, convenient, and gets me out. You might even consider getting a small dog to accompany you.
7. Do you feel that your new pain doc is listening and ready to work with you? Or did he or she kind of hurry you out with a prescription? If you do go back to discuss alternate treatments, have your ducks in a row as much as you can: know for example that the Arthritis Foundation says TENS units can help arthritis pain, and introduce the topic that way so the doc knows you have been doing some homework. “They say this, do you think it would be worth trying for me?” “If not, why not?”
There’s no need to be challenging, they hate that, of course—they do know a lot that we do not, and that’s why we’re paying them, but sometimes they do not bring that knowledge to bear on every case, or they may even be unaware of some alternatives.
I have gone on at some length, hoping that there will be at least one thing in here that may help you in your situation.
I wish you the very best, and maybe you’ll let me know how it is going.
nosleepingdog
Hi again NoSleepingDogs,
Well, after two weeks of trying the methadone, I am getting REALLY discouraged. It doesn’t relieve my pain very effectively (if at all!) and now I get headaches, heart palpitations, and dizzy spells. I called the doctor’s office and his nurse informed me that I have to “give it more time”. Two weeks isn’t enough time? I am seriously considering going to a different pain specialist. BTW… I have tried a TENS unit, with no success, I swim almost every day, and we have a hot tub which I use daily. I also try relaxation techniques… I realize that nothing is going to completely alleviate my pain, but now this “new” course of treatment (methadone) is so unaffective that I am back to waking up every night on the hour in pain. Arrrgghh!!!!
KC,
Sorry not to have responded sooner. I’ve been looking online for resources about chronic pain and families. What I have found so far is uneven, but each one has some different points to make. Here are some links:
http://www.nationalpainfoundation.org/articles/488/chronic-pain-and-relationships
http://www.nationalpainfoundation.org/articles/487/chronic-pain-and-parenting
http://www.nationalpainfoundation.org/articles/108/chronic-pain-and-family:-interview
http://www.nationalpainfoundation.org/articles/109/family-matters
Another thing that might help is keeping a pain journal
http://pain.about.com/od/livingwithchronicpain/f/pain_journal.htm
This can provide a more objective way of tracking your pain, what is associated with better/worse, and so on. Doctors appreciate this sort of thing and even in talking to your family it may help to show them that the pain is never absent, something that is hard for those around us to realize.
I have some templates for a pain diary that I will post tomorrow.
Methadone not helping…I am really sorry to hear that. It is less helpful than opioids? Have you discussed alternate possibilities with your pain doc such as TENS units? sorry if you already told me this. Obviously there’s no reason at all to continue taking either synthetic opioids (methadone) or regular opioids (morphine etc.) if they do not work. But there are different formulations that work differently, e.g. fentanyl patches, which are expensive and abused so some docs are reluctant to prescribe them, but I am told they often work better than pills. It all depends on the type of pain.
Also there is increasing research now on how continued pain actually becomes a physical problem itself, causing changes in the brain, and often making the individual more sensitive to pain. This is perhaps something to share with your family, I’ll post some links to articles.
I’ll have time tomorrow to get together more about this and will try to get a post up & also send it to you.
HELLO,
MY NAME IS AMANDA AND I HAVE BEEN TAKING TEN METHADONE A DAY FOR 2 YEARS IM TRYING TO KICK IT AND ITS SOOOOOOOOOO HARD AND NO ONE CAN UNDERSTAND OR FEEL MY PAIN BUT ME. TELL ME PLEASE HOW TO DO IT RIGHT!!!!!!!!
amanda,
My experience, described in the post, was that I could not get off methadone on my own. My pain doc would not help me, in fact denied that there was anything to it—I wasn’t having withdrawal, it was all in my head. When I switched pain docs, for the sole purpose of getting off the methadone, I found one with experience who told me the truth about how hard it was to do, but that he could help. A short course of morphine while the methadone got out of my system, other medications to help me sleep when I could not, something for nervousness (which I never had to use).
You’ve got to find a pain doctor who will help you through this. One source of a referral to a good one is to ask a pharmacist, or another physician, that you trust “who does methadone withdrawal?” As I said in my post, I was told it was harder to get off of than methamphetamine or heroin. And if you feel the pain from whatever your ailment may be, is going to be bead, talk to the pain doc about options for treatment after the methadone is done with.
You can do it, with the right help.
Amanda,
How is it going? Have you found a dr to help you with this yet? We’re pulling for you!
get liquid methadone from Dr and go down 1 mg per week. I was on 30 mgs
and took my time and got off
10 is nothing. I was at 105 mg and did a rapid taper while pregnant, that was hard, by the time I was down to 10, it was a breeze. Just do it slow, go down 1 mg every 1-2 weeks. When you are down to about 2 mg, all the withdrawal you think you feel is all in your head. Good luck Amanda, you’ll do fine
Really no, its not in my head at all. The first bit of taper was not too bad, and I actually felt less pain and had less sweating. This last three weeks coming down from 3/4 of a 5mg to nothing has been pretty bad, even with vicodin my pain clinic gave me to help. Certainly eberybody’s different.
Yes you’re right, everyone is different, I did mean by the time i was down to 2 mg, it was all in my head, which is a big jump from 10. I was just giving you my advice on what worked for me.
Hi, I just ran across your post at a important time. I am still hanging on to my NASIDS but my VA Drs. are afraid of kidney and liver damage I am being encouraged (strongly) to take opiates /methadone for my cronic pain. . I am willing to try just about anything other than Methadone hoping physical therapy/Acupuncture and NASIDS will help. Wish me Luck I have been going through this since 1984.
Yes, I think it’s a wise decision to try alternatives first. With chronic pain, probably nothing will give you 100% relief but we get pretty tough after dealing with it for a while, and even a 50% increase can be enough to let you do more things, and stay off the opiates & methadone. It’s a hard choice between NSAIDS & opiates, your drs are right to fear the liver/kidney damage. I do wish you good luck!
My pain specialist changed my medication. He took me off the methadone and put me on 15mg twice daily morphine, and 5 mg percocet for a breakthrough.
This works MUCH better and I no longer have headaches and heart palpitations.
KC,
Glad to hear this! That is really good news. Now that you are feeling better keep pushing the envelope on doing a little more physically, to stay in better shape and flexibility; that will pay off as inactivity that we get into, when in a lot of pain, ends up causing more pain.
WOW! Your story is amazing. Chronic pain and the meds are definitely something you have to experience to understand. I have major chronic pain in my lower back. I have been on opiates now for 10 years. I am 56.
After 9 years I lost my doctor and experienced the nightmare you talked about. Just as I thought I was going to have to go cold turkey, (Which scares me to death) I found another doctor to treat me. To write my scripts. I am on a large dose of dilaudid and oxycodone. I hate the meds and the control they have over me, and the fear of running out etc. but have to admit they work. Well, I think it has finally happened. I think I have lost my insurance. My two scripts cost around $1800 a month. My doctor told me to research methadone for chronic pain. He told me it was very effective for pain and was very cheap. I was shocked because I thought methadone was strictly for junkies to get off of heroin. So far I have read conflicting reports on methadone as a chronic pain med. and then I read your site and am more confused than ever. I guess my main question is does it work for pain?
It seems after much reading that methadone is harder to get off of than opiates, and that is really scary. I would like to get off it all, but I honestly can’t move with out them. However, because of this insurance nightmare that just surfaced, it looks like methadone is next regardless. Since you have done them both, which is easier to get off of, the opiates or the methadone? And once again, does methadone work for pain? Boy you sure hit the nail on the head about how society looks at all of this and how the doctors make you feel. This guy I have now seems to know what he is talking about, he knows more than all of the other doctors I have seen put together and he says it (methadone) is great for pain. You seem to answer all of the questions people ask you, I’ll be looking for your response. Thanks a million,
Chuck Graham,
Williamsburg Va
Chuck,
I’m sorry you’re in this terrible situation. But maybe there are more choices available.
First, methadone does relieve many kinds of pain effectively. Not all. For example, the pain I have from fibromyalgia is not affected. But for your back pain it would probably work pretty well. The down side is that methadone is harder to get off of than the other opioids (including morphine, even heroin) according to my pain doc, and as with the other opioids, toleration develops over time so increased doses are needed for results. It also has effects on one’s energy, thinking and memory, personality, etc., as well as the “not in control” knowledge, that you must have this drug.
I started on opioids when prescribed morphine for disabling muscle spasms in my back and it did work; later I was switched to methadone. But what worked better for me was a nerve block that allowed muscles clenched for over 10 years to unclench, and allowed me to move enough to do exercises the doctor recommended. At that point I should have gone off the opioids, but I had to change doctors, was dependent on the drugs, and thought it might be helping the fibromyalgia pain. The new doctor was the one I describe in the post who refused to help me get off of methadone, denied its severe withdrawal effects, and then finally told me he was taking me off it abruptly without offering any help.
While methadone may be the immediate answer for you, be sure you have explored all the alternatives that might replace it, such as nerve blocks, TENS units, even things like physical therapy. There are more such treatments that I don’t know details of but your pain doc should.
Doctors do not have much knowledge about alternative treatments such as physical therapy, but having just seen my husband benefit from the expertise of a really good PT, I know how much that can help. My husband went through 2 knee replacement surgeries on the same knee because the first one was badly done, causing over 2 years of pain, and stress upon the other knee. PT after the surgeries concentrated only on the knee, but this time he went in and listed the parts that hurt, got a complete evaluation of his joints, range of motion, posture and walking stance, etc., and they worked on all of that gradually so that pain from exercise was minimal. After long term pain your body can be like a structural expression of the pain, showing how it has tried to adapt and shift stresses to inappropriate joints and muscles. Some are overworked, others are atrophied or frozen in pain. The same thing was true in my case after the nerve block, when I had to gently stretch and strengthen muscles that had tightened up (to prevent further injury) many years before, and stayed that way.
So regardless of what pain treatment you have, at the appropriate time I would recommend seeking out a PT who can evaluate your entire body, and who will work with you in a way that you find encouraging and positive. Having lost your insurance, you’ll need to look at alternatives, even Medicaid and/or Social Security Disability if you are unable to work.
And also discuss with the prescribing doctor specifically what he or she will do when the day comes that you want to quit taking methadone. You will need expert help and prescription medication to get through the withdrawal itself. I needed morphine for a few weeks to substitute for the methadone, meds for sleep after the initial two weeks when all I did was sleep, and the doctor was also ready to give me meds for nervousness and other withdrawal symptoms. Before you begin to take methadone, be clear on your doctor’s knowledge and policies about this.
You have dealt with this extreme pain for a long time, so you may be all too familiar with what I will say next. We who have chronic pain need to look at it as a problem to be addressed from more than one angle, and count it as success if something we can do will reduce the pain level even 10 or 20%. Not that you stop there; my idea is that we put together a combination of things that help with the pain, and help us live our lives better with whatever pain remains. No silver bullet approach, no expectation of “100% relief or the method is a failure”. The mix varies for everybody, and can include medications, exercise, coping mechanisms (avoid what makes it worse, change your attitudes, change how you do things, get help), working with those around you so they have a better understanding and are more supportive, even meditation and relaxation. Anything that helps, keep it!
For right now, though, you must replace your too-expensive meds with something cheaper before you can explore alternatives. Just don’t stop after doing that. And, if you live in one of the 14 states that have legalized medical marijuana, consider that too; it helps a lot of people with pain including back pain. (Not me, unfortunately, since I do live in such a state.)
Good luck with this, and let us know how you are doing. I wish you the best!
Thanks for your input, I really appreciate it. You know as well as I do how limited the resources are out there for this, even though it seems that thousands and thousands of people are going through it. I will discuss this with my Dr. of course but I think I am just going to end it. Even though the thought of cold turkey frightens me to death, the worst is over in a week or so. And like you said, the methadone will only help for a short period of time and from what I have read, getting off of the methadone is even harder. The pain, well I guess I’ll just have to deal with it. I will ask for prayers from every one, and I will do the same for you. What a nightmare this is for us all. I have enough meds to last another week or so. I will keep you posted. God be with us all. Indeed Faith is the most powerful thing I have ever seen or experienced in my life.
Chuck,
Gradual withdrawal is a possibility too, that you could discuss with your doctor. Tapering off, rather than stopping abruptly.
Good luck—our thoughts are with you. Keep us posted.
Hi,
First Id like to thank NOSLEEPINGDOG for this wonderful site, along with the article on “nerve pain”. A perfect article, as it closely describes me. This is strictly my opinion, based on my own personal experiences.
I am 47, diagnosed with Fybro, and have been in chronic muscle/nerve pain for 7 years. Like most of you, I have been to various doctors, all of which, believed I was either mentally deranged or a drug addict. I lost my career as a paralegal, my husband divorced me within 6months of becoming ill, lost my home, and all of my friends abandoned me. I was left with a car, 2 children and no income. My children and I, squeezed ourselves into one small bedroom at my parents home. I couldn’t win for losing and the odds where completely against me. At the age of 40, I lost everything I worked so hard for and was completely disabled in the severest form of pain. God was with me tho! He gave me caring parents and ONE doctor who stuck by my side, helping me thru it all, despite every medical test saying, “I was perfectly healthy”. The rhumetologist told me, “I would be in excruciating pain the remainder of my life and there was nothing anyone could ever do for me.” A pain management doctor, hinted by informing me of a woman who saw Dr. Jack Krovorgian to help her “end her Fybro pain”. The psychiatrist told me I needed to become one of those individuals who could meditate and take their soul out of their body, in order to, acquire pain relief. Ya! Talk about depressing!
I would be happy to describe the severity of the pain I suffered, the varied symptoms, medications, and horrors I’ve been thru, but it would be to long of a post. Lets just say, I still have no idea how I survived the first four years of my illness. Most of what I remember is PAIN, PAIN, and more PAIN. I felt like I had stood in a camp fire for years, unable to move, flames engulfing my entirety, while burning pain scorched my very soul. Not even the strongest pain medication would touch me. After a few years, finally methadone relieved some of the pain. Thru time, the pain decreased enough to function. I have never been pain free nor med free, but I finally found relief. Currently, my pain has reduced even more, thus I am looking into a different medication, one which is more accepted by both doctors and society.
I took 20 to 30 mg of methadone a day, plus Lortab 10’s every 4 hours. I withdrawal off of methadone twice on my own, so as not to add onto my methadone intake after my body became immune. I had no craving for methadone, but suffered flu symptoms such as no man has ever seen. I had to change clothes every hour, as my clothes where literally drenched in my own sweat. I went thru it for about two weeks, but it worked, and once again I was able to enjoy pain relief. Recently, I was taking 10mg of methadone a day, reduced it to 5mg with no signs of withdrawal, then down to none.
Here is a list of side effects I experienced. The pro is simple, pain relief, as it was the only med that relieved my “nerve pain”.
As nosleepingdog states, if you have a choice and/or have found another med that will provide you with pain relief, methadone should be your LAST choice. For me, I had no choice, so I have no regrets, as I got my much needed pain relief thru methadone.
SIDE EFFECTS I endured from Methadone use:
1) Destruction of teeth due to dry mouth.
2) Insomnia and horrific nightmares “nightly”.
3) Behavioral/Mood changes such as Paranoia, Massive Depression, Anger, and Over-Sensitive emotions;
4) Blood thinner—For females, menstrual cycle can last up to 2 weeks, severe heavy bleeding, with forced sleep up to 3 days straight. Female organs can become sore during intercourse causing pain similar to a urinary track infection. Eventually, blood can be found in your urine;
5) Additional fatigue, loss of energy, excessive sleeping;
6) Hot and cold flashes;
7) Headaches;
8) Lower blood pressure—Ive always been funny about blood work, but since taking methadone I have not only passed out, but have stopped breathing on a few occasions;
9) Don’t get caught driving a vehicle or you will be put in jail for driving under the influence. The police department does not care if its prescribed by a doctor or not.
10) Society does not except it and will consider you a meth addict. People have only been taught that meth is a street drug used by addicts or a drug used to help heroin addicts withdrawal. Most do not know it is a prescribed drug for severe pain;
11) Massive constipation. I’m lucky to go once every 2 to 3 weeks and nothing works. When I do, its solid as rock, and I can feel the scraping pain in my back as it moves down the intestine. I then have to take an anti-inflamitory to calm the inflamation and pain caused from the movement.
12) Anorexia due to loss of appetite. I do not get hungry, so I have to remember to eat.
13) Anxiety;
14) Difficulty focusing and remembering;
15) Procrastination due to lack of energy;
16) Blurred vision;
Physical Therapy is very important, and should be done daily, thus I prefer to do mine at home. So, I found a wonderful site Id like to share. Its the best “trigger point chart” I have ever encountered. It not only shows you the various trigger points in your body, where the trigger points are located, but it also shows you where the pain is for that specific trigger point. Using this chart, I found my sciatica is being caused from a muscle called the piriformis muscle, which runs from hip to hip, overlapping the sciatica nerve tenants, also known as piriformis syndrom. I also found, my leg muscle pain is being caused primarily from the gluteus minimus muscle. (Damaged caused from working at a desk job for 24yrs) These trigger points appear to be causing or not helping, the knotted muscle pain in both legs, sciatica in both legs, both leg muscle are shorter then they should be, hip pain, and buttocks pain, of which I continue to suffer from. I have learned, when muscles are knotted it causes other parts of your body to become off-balance, including your spinal cord, thus causing additional problems/pain.
http://www.triggerpointmaps.com
I have since gained more energy, additional strength, and have found my pain to decrease some by using a few tools. Here are some of the things I do from home, again, this is based off my experience, but one I felt I should share. Please, do not use these without consulting your doctor. (1) I purchased an “inverse table” for $89, to re-balance and stretch both the muscles and spine. Like any stretching, I did feel additional pain when first using it, but the muscles began to stretch. My mother thinks I got taller. lol Who knows maybe I did. (2) I do not like going to the gym and walking does not provide enough exercise in the right places. So, I purchased a WII game. Wow! A WII game really does give you alot of exercise and you have so much fun using it. You forget you are using your muscles, so becareful on how long you play it. You also gain kudos from your kids and/or grandkids. lol I also purchased work out videos with the WII game, including the balancing board. The balancing board, lets you know if you are in the right position, very much like an instructor would. For the moment, I mostly work on the trigger point areas, which appear to be causing me the most pain. (3) I also purchased a tennis ball to massage the trigger points. While laying on the floor, I place the tennis ball under the painful area. Slowly and gently, I move my body around, allowing the ball to massage the area. Please becareful not to do this for to long, trigger points are exactly that, trigger points which can cause additional pain if massaged to hard or for to long.
Sorry for the long post, but I hope something I said, will help, as it has me. 🙂
The personal account of methadone withdrawal is almost exactly what I experienced! I am a woman with an injury to my neck and was put on METHADONE for pain! I acquired firbromyalgia about a year ago and after being on the methadone for over 9 years, decided to stop taking it! I got sick of the begging and being made to feel dirty like I was some kind of Methadone whore kissing up to my dealer for another fix! That is how my doctor made me feel! Well I did not go off it gradually with any help from a professional, I went COLD TURKEY!! I DO NOT recommend it at all! But it was like swimming halfway across an ocean and knowing that if I keep going I will be in civilization! Why would I swim all the way back just to be on land?
Anyway, I know how painful it is to go through withdrawals now, and that initself is incentive to never put another methadone in my body!
I am about 7 weeks into my detox and truthfully it is not over yet. I still have alot of bone pain, and fatigue, but thats about it. When I get back to my full self I am going to celebrate so much! My husband says he loves seeing me awake again. I do to! Hang in there everyone! We are All Awesome!!
Dear Kathy (who posted on Thurs. Dec 2nd at 8:22 pm):
Thanks so much for your post. Everyone’s imput helps and everyone’s story relates to my own in some way. I haven’t posted in a while, but if you are interested in hearing about my story, look me up in the postings under my name: kelly p.
I have a couple questions for you. I am rather surprised and impressed that you were able to quit methadone cold turkey. I wish I could do this, because like you, I am tired of going to my Doctor and feeling like a junkie looking for her fix and quite frankly I don’t want to ask my doctor for another thing. I have told her 4 times now that I want to get off of methadone and have tried to wean off it, but each time I can barely leave the house and I am only weaning myself by 5 mg, from 50 mg to 45 mg. How then, am I supposed to go from 45 mg down to 0 mg? My Doctor continues to tell me that Methadone isn’t hard to get off of if you just wean yourself. I know I have to see another Doctor, but my fear is that I will hear the same thing over and over again.
So, as for my questions for you…how many mg of methadone were you taking before you went cold turkey and did you wean down at all? Were you able to do anything during the first few weeks? I have a 2.5 year old daughter and am a stay at home mom, and I do have some help from my parents when my husband isn’t working. Still, I am a very busy stay at home mom that sort of takes care of everything in the household and the thought of not being able to move for several weeks scares me. But, it is doable if I can prepare for it and as long as it is temporary and it gets me off of this drug. The good news is that I have only been taking methadone for about 18 months. But, I have not gone a day without it in my system. I have pain issues, but I have several other things I do to manage my pain and at this point, I would rather live with my pain than live with the side effects of Methadone.
I appreciate your time and any additional information you might be willing to share that might help prepare me if I choose to go cold turkey. I know you are not recommending it and another thing I should mention is that I am on a very long waitlist to see a Pain Management Doc who might be helpful with providing help to get me off Methadone. Someone who will at least acknowledge this drug is terribly difficult to get off of. Now what doctors are saying is that it is only difficult to get off of if you are on it to get off of heroine, but not if you are taking it for pain. My question is: how the heck can you body tell the difference?
Thanks again and hope to hear back from you or anyone else who might be reading this with information that may be relevant.
Wishes for a blessed holiday season,
kelly p.
Once you start noticing the reduction of side effects, knowing others wont see you as a street druggie, etc., it gives you the much needed strength and hope for a better life. That alone, will keep you pushing thru the withdrawls, despite any struggles you may endure. Remember withdrawls are not forever, its temporary. Personally, I thought of my kids, which helped get me thru, as it wasnt just me who had to cope with the many side effects, my kids had to also. Don’t let methadone destroy your life, as it did mine. My husband, knowing the severe pain I was in, still considered me a drug addict, simply because it was called “methadone” aka “meth”. He divorced me, informing the judge I was a drug addict. My father told everyone I was a druggie. My friends abandoned me. I was left with no emotional support and judged before I had the chance to introduce myself. I was treated like a known criminal! As my kids got older, watching society judge me as a druggie, their respect towards me declined. I still endure massive pain, but at least I can hold my head high and not be judged as a criminal.
Kelly, you are taking a very high dosage, as I did 7yrs ago. Going cold turkey, I was unable to do anything, but had parents to watch over my teenage kids. Due to the severeity of pain, and doctors wouldnt prescribe anything else, I had to get back on it. I did this twice! Because, you have a small child to take care of, I would recommend trying to reduce your intake by 10mg’s. If your taking 20mg at night and 20mg in the morning…..try taking 10mg at night and 10mg in the morning. If you can handle the pain once your withdrawls have subsided, then reduce it to 5mg at night and 5mg in the morning. If your pain is bearable, then stop taking methadone entirely and seek other pain relief, even if you have to see another doctor to do it.
Good luck and Happy Holidays to ALL!
Dear Pam,
Thanks for your reply and to your answer to my question specifically. I like the idea of weaning down more drastically from 40 mg to 20 mg and 20 mg to 10 mg and so on. The only question I have for you that you may or may not be able to answer is how long do withdrawls typically last when weaning? I have heard up to two months? Or is that just when you go cold turkey? I know each individual case may be different, but it would be helpful for me to know how long withdrawls might last if I begin to wean in large increments.
Thanks again for your support. We all need each other. Congrats on taking back your life from this deceptive drug. I hope your family is now giving you the credit that you deserve.
Best wishes for a warm and blessed holiday season,
kelly p.
Hi Kelly,
Based on my experiences, going cold turky is extremely difficult. I only went 2 weeks, having to change my clothes every half hour due to heavy sweating, before having to get back on, cuz my pain was so severe. Thus, I don’t know how long it takes when going cold turkey. However, I do know, if not for the severity of my pain, I would have got off the first time I went cold turkey. I have found it to be true, its not the withdrawls that stop you from getting off, its the physical pain from the injury which is the problem. Thus why I mentioned, if the pain is bearable keep weaning off. Weaning was much easier. Each person is different, so wean yourself off based on your own descretion. I have been off methadone completely for 3 weeks. During the weaning process, I noticed little withdawl symptoms, some sweating, slight headache, caught the flu due to my immune system having lowered, and coping with my fybro pain. Not once, did I feel a craving for a methadone fix. (I smoke cigs, so I know what its like to crave a chemical). After being 2 weeks off methadone, the only withdrawl I noticed, was the chemicals in my body trying to re-stablize. Its not something you physically notice, its just something you know. Similiar to pregnancy, you have little to no symptoms, but you instinctively know your chemicals are changing. Again, I focused on the excitement of being rid of methadone, not being judged as a criminal, having hope again as depression eased, seeing other side effects dimenish, and mostly seeing my kids light up as my mood began to stabilize. I was so happy and focused on the good things, I saw the slight withdrawls as a temporary obsticale….similiar to having a bad cold or slight flu. Not a single withdawl symptom was strong enough to stop me from living life, on the contrary, I was to happy to care. You should notice diminishing side effects each time you reduce your med. You might even be surprised at side effects, you didnt realize you had. Each one you notice, gives you that much more determination to get off. Since you have family support, ask them to help point out the good things, while weaning off.
Now that I am off, I realized even tho the methadone controlled my muscle/nerve tendent pain, it was actually inducing pain. One of the side effects is muscle pain. Plus, the nightmares, mood swings, depression, inability to focus, all caused muscle stiffness, thus adding to my pain. In many ways, the methadone prolonged my fybro. In the 2 weeks I have been off, my muscles have relaxed, taking pressure off the nerve tendants, thus no more nerve pain. My muscles are now healing! While weaning, you might want to drink alot of gatoraide. Despite my doctor being mad at me for getting off the methadone, he did tell me the electrolites help keep your immune system up, helps with dehydration, and it helps heal the muscles. A second doctor confirmed it many years ago when I had a horrific flu and almost hospitalized for dehydration. He gave me a choice, an IV or gatoraide. I took the gatoraide and began feeling better the following day.
I hope that helps some. Good Luck! I know you can do it, for you and your family. ((HUGS))
I have been on Vicodin ES for years for back pain. Now my doctor decided I shouldn’t take pain pills no more because in the long run they can cause damage to different organs. So, she asked me if I was willing to try something else. I agreed. She then put me on Methadone. I haven’t had a pain pill in days. Yes, the Methadone helped my chronic pain for the 1st few days, after that, I felt like a zombie. My scrip was written for 10 mg. I was persribed 1 half 3 times a day. That lasted a week, then I was feeling sleepy thru the day, could not keep my eyes open to do my job. I called her and asked if it’d be okay to take 2 halves twice a day. She said fine. That still didn’t work, I was still in a zombie-state. Then they weren’t working for the pain. The Vicodin is the only thing that took the pain away and I was able to function normally and do my job. At the time, I was taking 4 Vicodin daily. I do not want to take the Methadone, I don’t like the way I function or rather, can’t function on them.
Sorry for not getting back to you in time to be of any help. My husband had shoulder surgery in December that went wrong and 3 more since then.
Vicodin ES has acetaminophen in it that can damage the liver and kidneys over long periods. (The liver damage is more likely if one drinks alcohol, too, which most of us do.) So your doctor is right about that. But your experience, and mine, is that methadone is not the answer.
Back pain can be from a multitude of causes. Some of those causes can be helped so that the pain is actually lessened, rather than just covering it up with pain meds. For my back pain what helped was a temporary nerve block to allow the clenched-up muscles to relax so I could stretch them out and strengthen them with exercise. That was after 16 years of living with the pain. Since then I find that walking is a good exercise to keep the back and other muscles strong (I should do more exercise! working on that). I think you and your doctor ought to go over the cause of your back pain and what other remedies there may be to reduce the pain so you could take less pain medication. It is not necessary to eliminate the pain entirely, but if you can find a couple of things that each reduce it somewhat, then you’ll be much better off. Maybe if you can do that and only need 2 or 3 Vicodin per day your doctor will okay that.
Thank you for your post on with drawing from Methadone. Because of the severe sweating along, is enough reason for me to get off it. I have been taking 10 mg twice a day and have now got myself down to 10 mg in the am and 5 mg in the pm. It has been a week today. I will say, however, I crave sweets more than ever. Since it has been a week since I cut back do you think I can cut back to 5 mg in the am now. I am so anxious to get off this. I have other pain meds for my pain. I had a failed back surgery in 2006 and now have 2 rods and 6 screws in my back. I will look forward to your answer.
Carolyn,
Yes, the sweating is more unpleasant than people who haven’t experienced it would think. I still overheat easily, maybe from fibromyalgia, but no longer burst into a sweat while just sitting down, since getting off methadone.
Not being a doctor I hesitate to give anybody specific advice. You don’t mention how long you’ve been taking methadone. If I were you I’d go by how I feel; try a further reduction and see. My experience was that I could gradually cut back to a very low dose without much effect but when I went off altogether I had complete sleeplessness and awful pain (methadone-related, not the pain I had taken it for). As you know from my post, I had to have a doctor’s help to quit the methadone but maybe your other pain meds will get you through, I certainly hope so.
If you do need help the dr who is prescribing the methadone and other pain meds should be able to help you, though in my case I had to find a different doctor. It is the doctor’s responsibility and he or she should have the knowledge.
And I can report that my craving for sweets that was so bad on methadone is gone. Used to be I couldn’t check out at the grocery store without picking up a candy bar, and in mid-afternoon I’d have a “slump” and eat a couple of them, but my candy bar stock sat untouched on the shelf for a year after the methadone ended, until I finally tossed them all in the garbage. Something to look forward to!
I hope this goes well for you; let me know. Afterwards I gradually felt better and better, and it is also a satisfying accomplishment that with so many things not under my control I did manage to do this difficult thing.
of all the forums i have come across, yours has been the first ive seen and said to myself, “this person knows what their talking about.” i have been on methadone since december 2009, and am still on it. along with myself, my fiance is also on it. we r both on 110mgs a day. i want to stop so bad, but the pain and discomfort is unbearable. if u could please let me know any and everything that u think may help, it would b greatly appreciated. like today i didnt take my dose till 1:30pm whereas i normally take it at 8am. and even though i just dosed, i feel terrible just because i took it 5hrs later than normal. would u recommend slowly lowering my dose by myself? and not telling my dr. just to ensure that i can control it? i am truly lost here, i mean, methadone saved my life from the heroin and all the other opiates i was doing, but i want my life back, free of dependance upon anything. please help.
Hi Bruce,
My name is Kelly P, and I have made several posts throughtout the last year or two on this website. I am NOT the author of this article; however, I thought that sharing some of my experience with you might be helpful. About 4 months ago, I made the switch from Methadone to Suboxone. The hardest part of that process was weaning myself down from 60 mgs to 30 mgs a day. In order to make the switch, you must be on 30 mgs of Methadone or less for about a month. It was hard, but SO WORTH the change. I had been on Methadone for over 2 years and was sick and tired of being sick and tired. I was afraid to tell my doctor that I wanted to get off of it for a long time becasue I thought she might wean me off too rapidily or take me off of it all together. And like you, if I took a dose even a couple hours late, physical and mental hell would ensue. Finally, I told my doctor that I wanted off of it because I had gained 50 lbs in 1.5 years, but after doing so my doctor continued to tell me that she thought it was the best thing for my pain and that if I did want to wean down, it is an EASY process. This was the same conversation we had month after month for the next several months. I would continue to come in and tell her that I could not wean down even .5 mg because of the pain and she would ensure me that it was what I needed. Each month I asked if there were an easier, softer way to wean down (even asking if I could be put in a hospital if I couldn’t do it alone) to which she would say, “that is for people who are addicted to methadone. Of course in my head I would say, “How could anyone taking this drug NOT be addicted to it…you literally become dependent on it and can’t NOT take it because your body gets so sick.” But, I was fearful that if I told her that I was, by all means addicted to Methadone, she would force me to wean down and/or off the medication…particularly because she thought (or was trained to say) that it isn’t hard to get off. Finally, what I call a “God shot” happened. I went to see a different doctor in the same office for an unrelated problem because my doc was out of town. This new doc appeared to be open and very considerate. I decided to ask him a question and what I said was, “I have been on Methadone for a couple years and really want to get off of it. Do you have an ideas as to how I might do that?” He replied, “Sure! I actually share an office with a doctor whose job is to gett people off of opiate medication.” So that day I made an appointment with this new doctor to discuss the possibility of getting off methadone. A couple of days later I was sitting in a room with this new Doctor, telling her that I want off of Methadone more than anything. She asked if I was taking it for pain. I told her “yes.” She then told me that in order to qualify for her services, I had to be addicted to it, not just taking it for pain. This led into a long conversation where I was completely open and honest about my long addiction to opiate medication. I told her that I was afraid to tell my Methadone doc, for fear she would just yank me off of it. This new doctor told me that I wouldn’t have a problem with the methadone doc doing that, but that I had to tell her I was switching to Suboxone myself. In other words, my Suboxone doctor wouldn’t do it for me. So that is what I did and it was a really was an easy process. Aside from the disbelief and frustration I felt when my Methadone doctor told me that “Methadone is a hard drug to get off of.” This coming from the same doc who told me month after year how EASY it was to get off of. I won’t go into her reasoning for the change of heart, but the bottom line is that I had seemingly found a way to get off of the Methadone. Was I thrilled that I was going to be taking a different OPIATE medication? No way. My goal is to be completely free of all drugs. But Suboxone is getting me closer to that everyday, whereas Methadone just kept pulling me further away from my goal. And it was so relieving to be working with a doctor now, who I could be completely honest and open with. Weaning down to 30 mgs a day of Methadone for a month was rough, but not nearly as bad as I thought it was. You’ll be amazed at how focused you will be, if you truely want off of the Methadone. I started off on 24 mgs of Suboxone daily and in about 3 months, dropped to 8 mgs. And I could have done it more rapidly, but I choose not to for various reasons. It is a fairly easy drug to wean off of. The beauty of Suboxone is that in most cases less is more. And even if I have to stay on 2-4 mgs daily for several months or years, my body really doesn’t feel like it is on a drug. Yes, if I go too long between doses, I tend to get that yucky all to familiar detox feeling, but nothing compared to what Methadone was like. I have energy, have not been depressed, feel better in terms of my pain and I am losing weight! And, I don’t crave drugs or alcohol at all. I credit that to Suboxone and my 12 step program and weekly counseling. So, in order to sum up all of this information, I will say that I think you need to go to your Methadone prescribing doctor and tell him or her that you have been stuggling with an apparent addiction to Methadone and that you wold like information on how to get off it. Tell him that you have tried weaning and it is impossible for you to even go down .5 mgs. If your doctor doesn’t mention Suboxone, ask about it. Don’t be afraid anymore to be honest about wanting to get help. Share your fears about feeling like you will be taken off of it if you ask for help. I think you will be amazed at how receptive doctors are to this situation because they are confronted with it frequently. If you want to, bring a parent, partner, or friend with you to support you. That is what I did. I brought my husband so that if I chickened out, he would be there to help me say what I needed to say. despite the fact that I told the Suboxone doctor that I was addicted to Methadone, she left it up to me to tell my Methadone doctor and to make the choice to switch if I so choosed. It wasn’t a case of, “if you don’t do it, I will.” You have to want to do it in order for it to work. It sounds like that is where you are at and it is exactly where I was 4 or so months ago. It was one of the best choices I have ever made. I hope this has helped you in some way or another and if you have any questions, please don’t hesitate to ask.
God Bless you and remember, you are not alone.
-Kelly P.
Bruce,
Kelly’s reply is a good one. (Sorry for my late reply; I’ve been distracted the past 2 weeks by another pain problem, my husband was in the hospital with immobilizing back pain; he’s home now with a long road ahead of physical therapy, not sure how much mobility he will regain and how much pain will persist.)
I would add a couple of things. Before you approach your doctor with the proposal that he or she help you get off of methadone, do everything you can to maximize your chances of success. If you used heroin, you will be tempted to go back to it. Your doctor will be concerned about that. Realize that being around people and places associated with past heroin use can trigger those old behaviors. Is your girlfriend on the same page as you are, will she join in this effort?
Can you put other rewarding activities into your life so you have satisfactions that would be damaged by returning to heroin or other drugs? If you don’t work, choose some volunteer activity that is meaningful to you, and commit to it; start before you go off the methadone (even if you have to take a leave from it due to withdrawal symptoms). Get those other pathways going in your brain, where you have other sources of meaning and self-worth, other people to care about, something that depends on you. This probably sounds rather corny but I think it is realistic. You’ve been on methadone for only a year and a half, so with luck your withdrawal won’t be that severe, especially if you can use substitute drugs as Kelly suggests. Still, life is not just about removing negative things, we also need positive things to keep us going and give us some direction while we are finding out “Who am I without heroin or methadone?” Your commitment needs to be strong, your support from others (doctor, girlfriend, and family or friends) also strong, and you need to build in continuing positive rewards that have nothing to do with drugs. Find activities that are really absorbing to you, so that time seems to stand still while you are doing them (these might be hobby-type things, or learning, writing, observing nature, whatever does it for you); and activities that give meaning to your life such as helping others, learning something new, preparing for a better job. These provide lasting positive rewards that get people through all sorts of crises.
I and many who have commented here can empathize with what you are undertaking, we admire your strength & commitment, and send our best wishes. Let us know how it goes.
I have recently turned 41 years of age. I have been on Methadone for the last six months; 10 mg every 8 hours. I have had none of the symptoms (thankfully) that you did. This is the 37th medication I have taken in the last 3&1/2 yrs for pain. It is the first one to work for more than 2-3 days at a time. I have been diagnosed with 5 bulging disks in the lumbar area of my back, disk degeneration & osteoarthritis in the middle of my back, arthritis along with joint fusion in the top of my back, arthritis & bursitis in both hips, carpel tunnel & arthritis in both hands & wrists. I have had all the shots & pain blockers in my back; all without success. I have been to physical therapy twice at two different places & even tried a Chiropractor. I am glad to have found Methadone & I am very thankful for it. I feel for anyone in pain & having trouble finding a doctor that believes their pain & finding medication that works; I pray you find the help you need.
Michelle,
Your pain is enormous, and I too am glad that you found methadone to work for you, and hope it continues to work just as well until maybe medical science comes up with something better. The complexities of pain mean that what works for one may not work for another, likewise with side effects. Everyone in pain needs to keep searching for one or a combination of things that provide them the greatest relief, without intolerable side effects.
I felt as though you published my diary when I read your personal account. I was looking for an alternative to methadone for chronic pain due to fibromyalgia when I found your post. Thank you for putting it in words what I have been trying to say to my doctor to help him help me! All my doubts about all these symptoms and side-effects being related are relieved.
I switched to a small dose of methadone after 13 years of vicoprofen treatment. For all the same reasons, after 4 years, I want to stop taking methadone. The fear and the difficulty is the withdrawal symptoms when the end dose is so small. I felt that I must be over-sensitive to not be able to completely kick it when the daily dose is reduced to 5mg a day. Thank you for having the courage to write this so that others who have experienced these things do not feel crazy or alone in this struggle.
You put down in words all the things I have wanted to discuss with my doctor. Wanting him to hear all of this and understand my desperate frustration was just not possible in a 20 min office visit for “med check”. Hopefully now, after I approach him with the main points in your letter as you have expressed them, he will be able to partner with me for a solution to detox and to future pain management strategy.
Thank you for giving me that hope and confidence!
I am 33 years old and have had chronic pancreatitis for the past 9 years, Im currently trying to get disability conisidering that all I do now is fight pain. Im among the 10% of people that they dont know why I have what I have but it never stops every body and their mother from telling me that its got to do with my diet. I can honestly say that I know for a fact that the only time diet has an affect is when I have a flare up that can last weeks. The affect is if I eat anything at all then omg talk about some pain. However my pain clinic has had me on everything from hydromorphone to fentanyl and nothing lasts very long so they prescribed me with the 5mg methadone. I have to say that when they gave it to me I wanted to laugh because I took it about 3 months earlier because of the occasional withdrawal sypmtoms of the opiods that I was on and it did nothing at all. Now they want me to take 1 every 12 hours for a week and then drop it down to 8 hours and basically I was wanting to know what duration is it typically before it starts to work because everything else I took kicked in around an hour and the fentanyl (fentora) was about fifteen minutes however they only lasted for a couple hours at the most. Its also a big difference from spending $200 a month to $5 for pain meds. Im gonna give them a week or so and if is doesnt help Im gonna raise hell about it because i’m absolutly tired of pain and then no life because i’ts impossible for me to work so then I have to depend on my wife to pay for my illness and on top of that I have no money so yeah life pretty much sucks right now!
3 months later, having reduced my dose in half from 20mg a day to 7.5mg -10mg a day, I am MUCH more comfortable. Weaning down was hard, even as slow as I did it. A few weeks of almost unbearable bone pain was the worst of it, when I went too fast. I tried to tough it out until I realized I had a better quality of life just taking the lesser dose. With no other solution in place for my Fibromyalgia pain, this makes the most sense for me.
The horrible sweating is much less, and related as much to anxiety as anything else, so I can calm myself or jump into the shower when it happens. Having reduced the dose as much as I can when I don’t have so much to do, seems to make my 10mg dose sufficiently effective on busy days at work. I am terrified of building up a tolerance again. I did this on my own before I told my doctor, for the same reasons and fears others have shared earlier. By the time I was ready to commit to the lesser dose, and knew I could do it, I told him I was doing so and he reduced my prescription and congratulated me.
This has worked well for me for over 2 months now and I feel SOOOO MUCH BETTER. Freedom of choice, about taking or not taking a larger amount on any given day, is a freedom I am glad to have back.
Thank-you for this article, it gives me time to think about other options for my chronic pain.
Gosh what a plethora of information..Ok I have chronic LBP, DJD, spinal stenosis, cervical fusion 2 herniated lumbar discs , and one in neck, I have taken Norco for several years with soma , up to 8 norco a day. Usually will relieve pain short term..Sometimes not at all. Hence fentanyl 12.5mcq patch which took the edge off. I went to pain MD this week, I was made to feel like a criminal, signing contract, subject to random urine tests, running curers report, etc..So i started methadone yesterday, 5mg three times a day..I feel like shit, and pain is really no better. If i stop now do i still need to wean? Of course I call MD and they dont call back but expect you to sign your life away and make one feel like a drug seeker..MD says norco is toxic to my liver and up to 8 a day, meaning the tylenol content which is 325mg and still under 4gm limit. I really dont know what to do. any suggestion would help, after reading i have made up my mind to stop methadone immediately..just worried that if i have been taking for only 1 1/2 days would i experience withdrawal?
Great article on the therapeutic uses of methadone in the treatment of chronic pain (a use that many are unaware of) and the potential downside to its use. Please know that I appreciate your article, and it has helped many people. I also have grown, over the years of being ill, to despise pharmaceuticals in general- and feel that I am almost better off with no treatment at all than what I have had at times.
I do hope, however, that you understand that not ALL experiences with methadone are negative ones- I think it is relative to the pain experience without it. I suffered for years before methadone was given to me as an option. It allowed me to have my life back, to be relatively pain free without the drowsy/sleepy effects of other narcotics. I sometimes taper my dosage down for a bit (this is something i do myself, because as you expressed I have a fear of being suddenly without my medication, or my physician suddenly taking me off of it), go thru a time of mini-withdrawals and misery, for the sole purpose of weaning myself down so that when I return to my regular dosage I will get back to those benefits that I obtained when I first started methadone therapy.
I’ve been diagnosed with fibromyalgia when the physicians couldn’t figure out what was going on, then later with multiple sclerosis, lupus, neuropathy, immunosuppression, blahblahblah for years- at least this physician actually offered me an option that has allowed me to work while being somewhat pain free.
I’ve taken methadone now for 5 years, 10 mg in the morning, 5 at night. I have never had the dosage increased.
I just wanted to point out that not all experiences with this medication are negative ones.
Sadly, as we read your blog and the comments, the same cannot be s aid about a medical profession that simultaneously pushes big pharma and yet treats its patients with disdain.
thanks again for such an informative blog. i hope you do not misunderstand my commentary as a criticism, but rather an alternative experience.
Fireside Academy,
Thank you for your comment; I’m glad to hear from someone for whom methadone has been helpful. You’re managing it wisely too. And you’re right, it is “it is relative to the pain experience without it”: if my pain had stayed at the severe level it was at when I started with opioids, then methadone might have been a positive thing for me. After my back pain was addressed with a nerve block and so on, the remaining fibromyalgia pain was chronic but not severe if I am careful.
Almost all medication for chronic conditions is two-edged, so that we have to choose—are the benefits worth the negatives. I’m adding a note to the beginning of this post, to that effect.
Best wishes,
nosleepingdogs
has anyone had experience using methadone for reflex sympathetic dystrophy (now called complex regional pain syndrome). My wife has suffered with that and fm for years, has had up dosage of vicodin with lesseing benefit. A new pain management specialist recommended methadone. My prayers and respect to all of you who suffer so and carry on with dignity.
Bob,
I hoped someone with experience would respond by now. Since I know little about complex regional pain syndrome I did some reading, such as this article http://www.rsds.org/1/publications/review_archive/CrucianiOpioids.html
which seemed encouraging. Another treatment, infusions of Pamidronate and Clodronate is discussed here http://painmuse.org/?p=54
One thing, which your pain doctor may have mentioned, is that switching from one drug to another for a period of time, then back, sometimes lets the patient get the initial level of relief at the original lower dose.
Best wishes to you both.
Chronic pain sufferers–Very interesting read!
Very informative read. I’m 23 weeks pregnant and have decreased my methadone from 105 mg to 15mg in that 23 week timespan. I am getting horrible back pain when i sleep, i wake up and my whole back is seized up. And the first withdrawal i always feel is in my legs. The constant feeling of having to stretch, only to be teased with 5 seconds of relief. Methadone withdrawal is more excruciating than when i gave birth to my previous son. I will not be prescribed anything else other than methadone, theres only one pain dr in town and its his way or the highway. I just feel stuck.
I’ve been on Methadone for 11 years now and i live in little rock ,Ar i lost my dr. or i should say i chose to leave cause i didnt like the way the clinc was runnin now im in a dilema cause i cant find a dr. that will accept medicare—-the ones that make u pay cash is the pill pushers in my book!!!! And my script will be gone in 3 days dont know what to do. I’ve had 4 knee surgeries
this is country boy still it cut me off——and i need my left on replaced i’ve als had a total right hip replacement which makes my lower back hurt cause i think my right leg is shorter the the left one. plus i had a defiralator inplanted in 98. i’ve looked and looked i guess i will go though the worst detox ever after 11 years of this. THANKS FOR LISTEN!!!!
Sorry to hear about your struggles countryboy. Be prepared for alot of sleepless nights. What dose are you on? The higher the dose, the worse the withdrawl will be in my opinion. Once i got down to a really low dose my body just would not tolerate it. Its been 2 months since i decreased to 1/10th of my original dose and my body still won’t adjust. Everyone reacts differently to withdrawl though, hopefully you’re one of the lucky people who get through it easily 🙂 I couldnt imagine going cold turkey, especially if you have a job that you need to survive.
I too have suffered from fibromyalgia for several years, and have run the gamut of pain meds, from lyrica to oxycontin and methadone. After starting to see a chiropractor for my fm, he told me to try Mucinex, 1200 mg extended release twice a day. This medication is sold over the counter for cold symptoms. What a miracle! This has made me pain free for the first time in years. Good luck to all posting here…there is help out there, if you look past Western medicine, who only look to heavy duty meds to treat chronic pain. Try Mucinex, Acupunture and Chiropracty.
This is the best write up I have ever read. I have been through many of the same issues, as I have been on methadone for almost ten years now. I have detoxed cold turkey twice & the first time the hallucinations were so severe I thought I was loosing my mind. I went back on methadone only because I just could not live with the pain any longer & I can not find or afford anything that works as well.
I have been on methadone for approx 8 yrs now.Before i was put on methadone i had made my way from oxycontin to 75 ml fentanyl patch.i lost 25lbs and weighed 100lbs when i finally had back surgery.after the surgery i was put back in the hospital for one week and weaned off of the fentanyl and onto methadone.I felt like i came out of a 2 yr daze.the fent was awful stuff and made me miserable and depressed.i started on 40mg of methadone every 8 hrs…and was not pain free but the pain was manageable.after 6 years i weaned down to 20mg every 8hr but cant seem to get below that without a great amount of pain and withdrawl. i have an ulcer so it is very hard to find a pain killer that doesnt eat my stomach.i also have fibromyalgia (diagnosed 20 yrs ago when it was rarely heard of,).Ive found that when i tell a “specialist” (and ive seen many) that i have fibromyalgia,more than a few have remarked “yeah,everyone has fibromyalgia”.It was a 10 yr long frustrating battle to get a diagnosis, and now treated,once again like fibromyalgia isnt real and im crazy or a pill shopper.Some doctors are real jerks. Im pretty convinced that Social Security Claims hires the biggest ones. i literally had to get a mental disability claim because i was in agony and on so many pain pills i couldnt mentally work.After getting Social Security i also got a change of insurance..Medicare…and got to see a good neurosurgeon who discovered that 4 of my discs in my back were gone…completely disinigrated! Ive had 2 surgeries in 5 yrs.Although it is nice to be vindicated, and now everyone knows im REALLY in pain, I would like to get off of methadone. I would never trade the time that methadone has given me to heal but the side effects start to get real bad after about 5 years on it.im having a hard time remembering words for things and i get lost in my own hometown! My thyroid is going haywire….i have hashimotos disease that “may go away if i get off of the methadone”.im not sleeping more than 4 hrs a night which makes fibromyalgia worse.im tired all of the time and im constipated.Now,out of the blue, im getting mindsplitting headaches every day at around 2-3 oclock.My dose is due at 3.It is very scarey to know that all of this could be the methadone but i cant get off of it.If anyone knows of a good alternative that is not narcotic let me know.(ive tried Cymbalta and Lyrica and Tramadol).Thanks!
I have been on for 13 years went from 200 mgs to 40 every 8 hours . I just can’t go any lower w/o that discomfort and panic. How can I find someone who can truely help me get off the rest. I am in florida
Does anyone have experience with the use of methadone in the elderly? My father is now 100…yes, one hundred, but has PAD in his left leg that is now exquisitely painful…like someone shooting him with darts. Sublingual morphine is not helping unless they completely knock him out…they want to try methadone. Ideas? Opinions anyone?
Well if all else has failed he could give methadone a shot. Who am I to talk though as I have only been on it for 2 months and am not quite sure of it myself. Don’t get me wrong it works better than anything else I have tried. Fentanyl made me sick, I’m allergic to morphine, percocet and norco have been my medication for the past 6 years. I know in the elderly the lowest possible dose should be given only once per day for the first two to three weeks. I like the information from these posts and it is my first ever to reply back on. I like the honesty of it. I have yet to find a pain management dr who doesn’t throw addiction in my face. My pcp is my prescriber and now my options are limited since I have no insurance at the moment. Hence the methadone. I don’t think I would have even considered it but the cost is way more reasonable.
I did a little research on methadone and the elderly. There was a nursing home director who was putting the residents on 2.5mg of methadone daily for pain management and it actually worked. They complained less of painful episodes slept better. I would think it could possibly build up enough to be toxic due to age related declination in health and organs. He would definitely have to have blood levels drawn on a monthly basis but it could work. 100 years is a long time to live surely he has been blessed with a long life and shouldn’t have to suffer. I am just not sure about methadone for the elderly. Have they tried other medications?
Susan…who is they? His doctor?My doctor is one of the few in our rural area allowed to prescribe methadone,fentenyl etc. These drugs are not normal narcotics and need to be monitored differently. I am on methadone and have to have an ekg yearly because it can have adverse effects on your heart. I have alot of pain but am only on 20mg of methadone per 8 hrs.This is a safe low dose. I think that the relief would be great for your father….it is to me.As long as he doesnt have any underlying heart issues and he is being monitored (more often then me) by a doctor who is an expert on these kind of drugs. (My doc is licensed for hospice care,which usually includes drugs for people who need drugs that people dont go on for more than a couple years).i was on fentenyl for a year until my back surgery….then weaned down to oxy then down to methadone. Methadone is considered a lower risk drug than morphine…and it does not knock me out.i can get out of bed and function….no running,lifting etc but at least im not in constant pain.Hope this helps!
I just weaned off Tylenol with codeine (Tylenol 3) after taking it for almost 20 years. It took me two months to get off it. I also have fibro, peripheral neuropathy, TMJD, degenerative disc disease, and osteoarthritis, mostly in my spine. So now I am looking for new pain mgmt. My neuro suggested a pain doc and spoke about methadone. Now I will DEFINITELY NOT be swayed into taking methadone. I will advocate for something else. Thanks for all the in depth info…everyone!
I have found this whole site on pain management very interesting. However, I am NOT convinced that Methadone is not the answer for many people. I agree on starting on low doses of anything and also using other techniques for pain management. I have taken low dose Methadone for a week and I almost feel normal again. But, then again…it all goes to pain tolerance AND how much pain you are in. And I would bet everyone who has posted here…no two “pain scenarios” have been the same. I have had chronic pain for about 13 yrs. for years I took two Ultrams, 1 Soma…4 times a day. And, no, I never needed to increase my medication until I was diagnosed with Lyme disease! There’s a new one for you..I already have Epstein-Barr virus for two years, with increased my fatigue and exacerbated my Fibromyaligia…which is OFF the charts. 21 yrs of heavy duty massage in Physical Therapy setting..plus neck fusion, which was fixed with micro-surgery, only to be ruined 7 months out when my car double rolled on a freeway and ended up on the other side. I have also had my low back scoped and decompressed by some bone removal from the vertebrae in the lumbar region. Also nerve ablation on neck and low back. Did any of you know that Lyme is the fastest growing infectious disease in the country? Hard to diagnose because it mimics everything: Ms, Lupus, Chronic fatigue, RA, fibro…HMMNN…interesting. You would HAVE to fina Lyme literate doctor. The others don’t have a clue, because Lyme has Many co-infections! Because of my IV treatments for this and high doses of anti-biotics, my chronic pain increased and I could not manage it with the same routine of pills…I had added some Lor-tab..lower dose. So, my doctor…who ONLY sees Chronic Care cases wanted me to try Methadone. I am not against it or freaking out like many on these post about withdrawal. I has given me pause to as how much of a dosage I will allow myself…and if I start feeling too weird of side effects, I back right off. Something I did with Morphine years ago after taking it for 3 days. Talk about being “out there”. But, I also believe I was NOT in advanced chronic pain at the time, and the morphine was too much for me. But, in a week of Methadone, I have felt the first relief of increasing pain for a year. So, I am not ready to throw Metadone under the bus yet. If you are in excruciating pain..um..that’s WHY you take it…duh. If anyone would like to see some eye opening film on Lyme Disease and the ravages and carnage it creates…sometime for years..before its figured out…check out the movie: Under Our Skin. And a shorter one called Lymelight. Oh, and yes, I suffer from depression. But, I was diagnosed with it WAY before chronic pain became an issue. But, since my pain has increased this last year, so did my depression! I do walk and hike steep trails with my dog. Some days I have to skip it. But, I was a pain free athlete once, so I believe in some exercise. But it is hard to get out of the house! Yours in health, Pam Green from Utah
has anyone tried Suboxine for the withdraw symptoms of Methadone I know some people who have sucsessfully used it to beat the withdraw symptoms…. as for me I have been in chronic pain for about 7 years and I have taken way to many advil I was planning on going to pain management until several people said due to a crack down by the dea and various law enforcement agency in my area that they will not prescribe any opiates. This is such a shame for those of us who suffer from chronic pain. I have severe joint and tendon pain in just about every joint in my body along with heel and foot spurs, I have not had a pain free day in 7 years. people who dont have chronic pain have no idea how it is to absolutely not be able to get away from pain..the only relief I get is when I sleep and it wakes me up every 45 mins to an hour. I am contemplating going to a methadone clinc and saying I am an addict to get access to the methadone but after reading this I am having second thoughts. I have to do something as I turned to the streets to get pain meds but its just too expensive not to mention illegal. I am taking 90 mg of oxycodone a day and getting very little pain relief. I dont want to be called an addict or pill popper but I have to get help for the pain before I go postal…I have to make a decision does anyone have any advice?
My husband received Suboxine to get off of Methadone with very favourable results. He suffers from a spinal injury from 27 years ago, so has been put through a whole range of medicine. Methadone although in the beginning worked it soon became apparent that it was not. It destoyed his body even more including doing a real number on his teeth and mind. To get off was even harder but with the help of a pain doctor was given Suboxine after he was able to get down to a minimal amount of Methadone. She told us that Methadone should only be used as a very last resort, that Suboxine is saver and works on a different principle than other medicine. He was precribed only long enough to get off of the Methadone, although the effects that the Methadone had on his body took well over a year to subside. He was only on Methadone for three years.
He also suffers from chronic migranes but those have also subsided with the use of the medicine that he receives now Nabilone which is the same basis as Marijuana he takes 6 mg at night and sleeps better is more relaxed and his headaches are fewer.
My husband is now looking and reading into Medical Marijuana as to uses and effects as it may be less expensive.
Mary that is great to hear, Suboxine is a life saver for anyone trying to get off opiates of any kind… I have been a life long advocate of medical Marijuana , I live in the state of PA and they are refusing to legalize it for medicinal use even thought there is ample evidence that it is very effective to combat many things, I was able to control my pain in the early stages with Marijuana but it is way past that now..I go to the Dr. tomorrow I hope I get the help I need
Mary,
Methadone does not rot teeth,nor is it the LAST resort! The last resort is what I am about to endure.Intrathecal priault pain pump.Check yourself.
Read about SUBOXONE.Listening to your doctor is more dangerous than suboxone/methadone/all pain meds combined.You must educate yourself and so to..your husband.
Doctors adore patients who are ignorant,concerning their own bodies…they can make more money/by seeing more patients. Good Luck,
Dan F.D. Maloney
ps I had 4 failed total spine surgeries and five others.Your husband on Methadone from an injury? Now that is wrong!
He never had surgery!!! Is this an insurance issue????
I also am on methadone 60 mg a day I have osteoarthritis and rheumatoid i have had 2 hip replacements severe scoliois djd of spine and 11 bulging disc they will not due back surgery . Im on the medicine 6 yrs Ive been on others, and was able to wean myself off I know ,my sex life is awful due to this med, I have to take something.Can u recommend anything less life changing, I know a low dose of moriphine will help withdraws, but do you think 30 mgs eill be enough open to advice. Thanks Lois
Wow. I am currently embroiled in a nightmare war involving Kaiser and the terrible doctors they hire. The decent caring doctor i had got transferred, and i found myself assigned to a new and awful excuse for a physician, one Aimee Packer Ostick, an ignorant, self serving, incompassionate, uneducated, arrogant, downright unprofessional unethical borderline criminal excuse for a doctor AND for a human being. I am 30yrs old, have had chrons disease since i was 7yrs old. I have, and always *have had, a very strange body that has weird/rare reactions/side effects/allergies/etc that for most people are harmless. So too does that include the fact i have, and always *have had, an almost superhumanly high tolerance to narcotics/etc. I have a naturally high tolerance, and a strange body chemistry that is different from 98% of the population. That is not my fault, i should not be penalized for how my body works. I am JUST as entitled to have my pain managed and controlled, and JUST as entitled to be able to function, to have a life outside of my illness and pain, to seek some semblance of happiness. But our miss Aimee Ostick just does not see itthat way, cannot grasp that simple concept, all she sees/cares about is “the amount the amount” NOTHING else enters her mind. Yes, i am on a very high amount of narcotic medication (dilaudid and time release oxycontin) yes, i get that doctors see that amount and get scared, but they need to look at the INDIVIDUAL patient case by case, to realize not ALL people fall within the same normal range, that for some, different than the normal amounts are appropriate for the patient when there are legitimate reasons as to why they recquire that amount. Again, i dont deserve to suffer just cause my body is different. The meds i am on manage my pain just fine, they allow me to function, to have a life, to have a relationship w a man i love, to maintain relationships w family/friends/etc. Without these meds i would have none of the above, i would be, quite literally, bedridden 24/7, crying, writhing, screaming in pain unable to eat, to leave my bed, to converse w anyone, NOTHING. That is exactly the fate miss Aimee Ostick would have me be in if she has her way. (Currently looking for a different doctor so i can escape Aimee and her
Malpractic, but that takes time and in the interim, i am at her mercy. She has most recently come up w a new bulls*** justification, trying to misdiagnose me w hyperalergesia to justify taking away the meds that allow me to live and have a life, and eventually get me onto methadone, which i will NEVER allow ANYONE at kaiser or anywhere, to make me poison my body w that because its cheaper for kaiser, its not my damn job to save kaiser money. Its fine if methadone works for some patients, but i am already ON the appropriate regimen for my individual medical needs, plus that i feel for me, personally, methadone would do harm to me and i have a right to not allow ignorant doctors to poison me w something so they can cut costs. Though its a moot point because i DO NOT HAVE hyperalergesia. I show ZERO of the signs, symptoms, or indicators of hyperalergesia nor have i EVER shown any (not that Aimee or the ignorant pain doc she sent me to after she coached him & biased him on what to say/think-which he openly admitted-, would KNOW if i actualy had ANY of the symptoms/signs of that, as they never bothered to ask me ANY questions, have a SINGLE conversation w me, NOTHING) she/he had her mind made up before even walking in the door and introducing herself/himself, all because of “the amount the amount” and just pulled this total BS hyperalergesia misdiagnosis out of her/their ass to justify her already decided opinion and agenda, zero regard for what is right for ME as an individual patient &what is medically appropriate for ME, NOR any regard for what she and her malpracrice and incompetence are doing to me my body and my health in the meantime, or the damage/harm she is directly &personally causing me. Chrons is profoundly effected by stress, and as you would imagine, all this BS shes putting me through is extremely stressful & i can already feel my chrons starting to flare up, so she is directly causing a patient to suffer bodily harm &to be a threat of continued and worsened harm, nevermind the stress of having only two days of meds left, and an ignorant self serving doctor who doesnt give a damn, and i feel so lost and terrified it seems no one in kaiser can or will help me, nor do any of them care, unable to find anyone who can be an advocate for ME the patient, and in two days i will be w out any meds. Left, i guess, to either seek out illegal drugs off the street (which i wouldnt have ANY clue how to do even if i wanted to)… OR, to instead opt for suicide rather than face the severe unbearable pain i will be subjected to as WELL as the withdrawals, if someone in kaiser doesnt step up &do their damn JOB & HELP me, the patient. This is just so so wrong that i could even be PUT in this situation at ALL due to uneducated uncaring doctors who care nothing for the human being whose life they hold in their hands and who instead serve only their own hubris and self benefiting agendas. Its NOT okay, it should be criminalized, sick worthless doctors like this should NOT be carrying medical licenses, have NO business malpracticing medicine on any living being, period, and if kaiser allows this, then THATS not okay either, &should too be criminalized. We, the patients, are REAL, individual unique human beings w lives &people whom we love & who love us, w hopes dreams hobbies goals etc, &we are ENTITLED to those things. We are REAL people whose lives these “doctors” are affecting-their halfhazard guesses &half-assed decisions have very real &profound consequences that the PATIENT is the one that will have to suffer from them. The “doctors” get to go home and forget ALL about those patients, those human beings whose lives &bodies they caused grave damage &harm to, forget all about all the uneccessary pain &suffering their arbitrary choices caused to real people, cause they simply dont care. They probably wouldnt be able to even remember a patient by name, or recognize a patient on sight even, cause we arent people. We are faceless nameless medical record numbers thats it.this is all just so wrong, immoral, unethical, just…. WRONG that they can do this to people and expect it to just be allowed and submitted to, cuz how am i (or any of us) supposed to fight an entire uncaring organization/hmo that cares only about the bottom line-money, &if an individual like me falls through the cracks, or loses their life, or is harmed/damaged/bedridden & *wishing* they *had* lost their life rather than suffer THAT medically sanctioned TORTURE, then thats just fine w them-they wont fret or lose a minute of sleep over it. It makes me shudder to think to myself &wonder, just HOW MANY patients do they directly &single handedly drive to the depths of pain dispair suffering &desperation thats ends either in: the use of illegal drugs, OR, the committing of suicide rather than live in bedridden unbearable suffering. HOW is this okay HOW is there not an advocate somewhere who exists to HELP patients, since the “doctors” DAMN WELL have NO interest in doing THEIR job which is *supposed* to be advocating for their patient/protecting them/standing up for them, but in kaiser these “doctors” do the opposite &show no desire to advocate for anyone but themselves their ego and the furtherance of their own (undeserved) careers & desires. So when our doctor personally directly fails us as a doctor and as a human being for that matter, what the hell are we to do? What recourse do we have, what options, what course of action can be taken to protect ourselves &our bodies from further imminent harm and damage? Who will help us? Or are we expected to simply lay down & submit & die?
Ok, so you need to vent, I get that. And doctors can be seemingly unsensitive and frustrating, but this is a forum supporting those of us dealing with treatment with Methadone. How is your rant helping us, or how can we help you, if you want nothing to do with the “poison” of Methadone? Perhaps there is a better site to address your problem with the medical community. I do wish you luck in finding an understanding doctor.
Missy, please do not address me in condescending patronizing manners. You obviously have nothing positive to contribute, so you shouldnt have bothered at all. Try having some compassion, understanding, and empathy. Instead of going into your OWN rant aimed at me. First off, my “rant” as you call it so inaccurately, was not a rant, nor was it about “needing to ‘vent.'” It was my situation along w just SOME of the background that goes along w it, so that my situation and my questions had at least SOME background & context, in case anyone who read it had any answers, advice, or anything helpful to me, which you obviously do not, but chose to respond anway, in a rude, apathetic, know it all tone i might add.
Second, this, as *I* personally understand it to be, is not MERELY a forum for the support of methadone use. It is a forum for pain patients, for the discussion of both the pros AND cons of the use of methadone for pain relief, the discussion of *alternate* meds & methods to treat pain other than JUST methadone.. …. I was *very* clear in saying that I do not deny, nor have a problem with, the fact that for some patients, methadone works for them. I very clearly said that for ME, & for MY individual body/body chemistry, MY individual medical situation &medical needs, that methadone would be tantamount to poisoning & harming ME & MY body &was wrong for ME individually, ESPECIALLY since I would be doing so only to help Kaiser cut costs, which is NOT my job & not *supposed* to be the doctors priority or concern either, and ESPECIALLY sine i am already ON the appropriate regimen of meds for ME that manage my pain & allow me to function, which as a human being, i am just as entitled to as anyone else. I never once said that methadone was bad or evil or poison to ALL patients, nor did i say it didnt help some people, i clearly said that it was poison for ME & would harm ME & was not right for ME as an individual. I doubt you even read my whole post cause if you did i find it hard to believe that anyone would respond the way you did w such insensitivity and lack of compassion, to someone in need, to a fellow sufferer of severe pain, to someone in dire need of help/advice on where i can turn to find someone who will be an advocate for me, the patient, & my medical needs instead of being let to fall through the cracks & have my life & ability to live & to function, taken away for NO MEDICAL reason, and need help getting pointed in the direction of someone who can be an advocate & help me through this situation in one piece as in two days i will have zero meds. If anyone *does* have any advice or suggestions of what i can do, who i can contact, how to find an advocate who cares about *helping* the patient, anything/anyone i can do or go to for help in fighting this BS im being put through by ignorant self serving doctors trying only to serve their own hubris and further their own selfish agendas, please let me know, i would be so utterly appreciative of ANY help/suggestion/advice, like i said, i feel lost and helpless, at the mercy of uncaring ignorant doctors and a huge corporation/hmo that doesnt care about the individual patient(s). Missy- you obviously are not one of those people that has anything kind, caring, positive, or helpful to offer, so please, do not bother responding to me again. If all you can do is be condescending and insensitive and negative there is no point in replying. I suggest you try to maybe learn to have a bit of empathy and understanding and kindness towards pain patients who are suffering and feel alone helpless and abandoned by uncaring uneducated arrogant doctors, instead of leaping into a rude insensitive offensive self righteous rant about how “this forum is to help patients who use or want to start using, methadone ONLY. If you are a pain patient seeking help but are NOT taking or considering taking methadone, then you are not worthy or deserving of any help/support/or advice & your suffering doesnt matter to me just because you use meds other than methadone & do NOT want to be put on methadone, youre of no concern to me, so go away & continue to suffer elsewhere.”—thats basically the gist of your comment as i interpreted it. Which is funny because this exact forum is in LARGE part what made me decide for SURE, among other reasons, that i would never ever allow them to make me, personally, take methadone.
Again- if anyone has any REAL advice/suggestions/help/etc, please let me know, it would be so truly appreciated, as i feel so lost and panicked and about to be w out ANY meds in two days.
Missy- please dont respond to me & keep your negative insensitive condescension to yourself as it serves no purpose and isnt helpful to ANY of us here. Again this forum is for pain sufferers/patients to find advice and support, to discuss the pros AND cons of methadone for pain, to discuss and offer other alternatives for those not wanting to use methadone/etc. This forum is not ONLY for patients currently taking methadone- i have read & followed this forum for quite a long time & never has it or anyone on it claimed that it is for patients currently taking methadone and ONLY them- NO ONE else is allowed to seek support here, thats just not true. Like i said it was actually because of this forum that i decided for SURE that methadone was not for me & that i would never go on it. That doesnt mean i dont deserve support/advice, especially since my issue and situation *is* very MUCH methadone related: having to figure out how to find help/an advocate to help me to fight my ignorant doc & protect myself from their malpractice & misdiagnoseses that have NO medical basis & simply want to take away the meds that work for me in order to cut costs and force me onto methadone because its cheap. Its very much a methadone related issue, a pain patient issue, and a pain management issue. This forum is NOT only for patients who are both currently and happily using methadone to treat pain. Its for discussing and supporting and helping people in the aforementioned ways as well.
But i thank you for your insensitivity and lack of compassion understanding or kindness, as a pain patient, im used to it, i just never thought i would encounter it HERE, in this forum that ive been a longtime reader/follower of, & has seemed to be full of kind helpful supportive understanding people for the most part. I guess theres always an exception, even in seemingly safe z& caring places as this, & apparently you are that exception. Please leave me alone and allow me to recieve any help/advice that anyone may or may not have to offer me, without further interference or self righteous, “for *current* methadone users ONLY!” Elitist attitudes, thank you.
Because i truly truly do need some help/advice badly, if anyone has any suggestions, it is much needed, thanks.
Thanks to all who have shared their stories. I have been dealing with chronic pain for the past 6 years due to a painful arthritic condition called Ankylosing Spondylitis, as well as Fibromyalgia. Early on my pain was primarily in my lower back, but now I also get severe pain in my neck, hips, knees, wrists…all of the joints. With the fibromyalgia I am very sensitive to touch so things like laying in bed are a nightmare for me. Severe fatigue is problematic with me a well. When I first started having pain, I was taking 7.5 mg hydrocodones about 3-4x a day but after about 6 months I was up to the 10 mgs. I never received much pain relief from this medication but the euphoric feeling it produced was a pleasant distraction from the pain. Also for whatever reason pain killers give me energy instead of making me tired, which was a welcome side effect for me due to the constant fatigue I have.
After a year or so I saw a pain doctor because my pain started getting worse as the pain pills were very ineffective for my pain, and I was having pain in other places than my back. Luckily i had a great pain doctor who was willing to help me find the best medicine for me. Just like all pain doctors, he wanted to do the injections, but they didn’t give me any relief. It is frustrating that these days most pain doctors will only do injections and not even prescribe medication, which I understand do to how much money they make, but for those out there like me who don’t respond to injection therapy, it makes it very frustrating.
Well this pain doctor switched me to fentanyl which I felt didn’t help much, time released morphine, as well as oxycodone. I also have tried Lyrica, Cymbalta, and Neurontin which gave me no pain relief and made me feel like a sluggish zombie. I took oxycodone for quite a while as that seemed to help the most with my pain, but as most of you know, strong pain killers like this also produce a lot of euphoria which makes it a very addictive medication. I ended up moving to Florida after being on the oxy for a while, but found out that Florida(or the are I moved to) was very hard to find a doctor who would help me. They all wanted to do injections and nothing else for the pain, and wouldn’t give me anything to help with the withdrawal pain to get off the oxy. I did it cold turkey and it was hell for about two or three weeks, but to those that say they can’t get off of it, its all about how bad you want it. At the time I was getting off of the oxy I had decided to just get off of pain meds completely because I was tired of being at the mercy of the doctor, and if the were going to fill my prescription or not. Sometimes I feel that dealing with my pain is a better option than dealing with being addicted to pain killers and dealing with the doctors.
Fast forward a year and a half, my pain is way worse that ever. I went a year and a half without any medication and just dealing with the pain. I would push myself and exercise, a lot of hanging out in the hot tub, and trips to the beach to relax and “get away”.
But now for the past month I have gotten on the hydrocodone again, which hasn’t helped much, so I went in to see a pain doctor in my area. I told him I wanted to try methadone because I have tried just about everything out there with only a little or no relief at all. I am going to try and take it for a month or two and see how it does with my pain, but if it doesn’t help me much I will get off of it and try something else. I am currently on day 3 of taking it at 5mg 3x a day which will go to 5mg 4x a day on day 5. I was also prescribed 15mg morphine ir for the breakthrough pain but have noticed no effect at all when taking it. Although only a few days in, I am actually getting a little pain relief in my back. Another thing I like about methadone so far is that i don’t get that euphoric blast like I do from oxy, which is what I don’t like because that is what gets most people so addicted in my opinion, and gets people drawn in to chasing the high and not combating the pain.
To those who live in a state where medicinal marijuana is legal I would highly recommend trying it out. If and when it becomes legal in my state, I will get off of this synthetic stuff in a heartbeat in lieu of that amazing plant. It does help for pain quite a bit, as well as cures or ails many other things, but being that it is still illegal in my state, I feel it is too risky to be using it. For the time being I will give this methadone a go. To all of those that are also suffering, I feel for you and hang in there. It is tough when those around us can’t relate because they don’t deal with the constant chronic pain, and don’t understand what we go through.
Brody
Again thank you. I am currently involved in a taper study for discontinuing opioid medications. I have experienced many of the same intolerable symptoms, from sweating, munchies, and vaginal issues that, neither my docto nor I, attributed to methadone use. I am so happy to read off your success. I am encouraged.
Hi for 27 years I was on Methadone, NO addition ‘why’ had no where else to go, neuropathic pain ‘full body’ man made not god given, “thanks Doctor” in public hospital whom although practising as a specialist NEVER completed his pract training ONLY theory. Oh, I don’t have two heads.
The author is totally off course.Why?I have had for failed major spine operations,achilles tendon surgery/,rotator cuff surgery/ulnar nerve transposition most recent total failure/.
I am prescribed 30 mg Methadone daily and i have no life.
Fibromyalgia/pseudogout in knees..constantly.
You have no business taking Methadone…period.You have not endured insults to the system{SURGERIES}or Cancer….I have……………
Myself,I never took any pills for anything until age 45 or so.
You,on the other hand have a “sissy” attitude.
Total neuropathic,mind crashing pain that forces one to live in one room.
I started to not only read your article but the responses, however I stopped, reason everyone responds differently due to not only dose, medical condition/symptoms etc and personal tolerance. Now I have said that, my personal experience I took Methadone (pill, not liquid) for 23 years I do not have two heads and believe still have all my faculties. It is very wrong to advise others based on one’s own experience. Finally, ‘if it works don’t try to fix it’, 23 years is NOT 3 or 5 Oh, I had both neuro and physical chronic pain and related disability, note I said HAD. Outcome that’s ‘another story’, but Methadone got me through.
Aussiere,
You must be a happy gentleman because ,no longer must you “ask” for a
drug{METHADONE} from the doctor/nurse/chemist or pharmacist and ready yourself for a condescending glance or stare…..My prayers for you in being free of it. Dan
Hello,
My girlfriend has been on methadone for over 15 years and had recently came off of it. its been about 5 months and she is having severe muscle pain and has been to doctors and not of them have helped or even know what to do for her. I am worried that she will be unable to handle the pain and have to go back to opioids or other drugs. does anyone have any experience with this and how long can this muscle pain last. she was originally give methadone as a maintenance for heroin and now all of the withdraw has passed and she is left with this muscle pain. does anyone have and ADVICE Please.
Actual topic,